Br J Cancer:三种靶向HER2的酪氨酸激酶抑制剂的比较分析
2021-01-28 xiaozeng MedSci原创
ERBB2/HER2(表皮生长因子2)基因在癌症中经常被扩增或出现突变。既往研究已证实了在乳腺癌和其他癌症中HER2的基因扩增以及蛋白质的过表达,并已开发及批准了许多靶向HER2的疗法。
ERBB2/HER2(表皮生长因子2)基因在癌症中经常被扩增或出现突变。既往研究已证实了在乳腺癌和其他癌症中HER2的基因扩增以及蛋白质的过表达,并已开发及批准了许多靶向HER2的疗法。
目前靶向HER2的疗法可大致分为三类:赫赛汀(曲妥珠单抗,Herceptin)和帕妥珠单抗(Perjeta);曲妥珠单抗emantasine(美坦新,T-DM1,Kadcyla)与曲妥珠单抗deruxtecan(德鲁替康,DS-8201,Enhertu)的药物-药物结合物;小分子酪氨酸激酶抑制剂(TKIs)。
其中,三种靶向HER2的TKIs,拉帕替尼(lapatinib,Tykerb / Tyverb)、来那替尼(neratinib,Nerlynx)和图卡替尼(tucatinib,Tukysa)目前已获得FDA批准,用于治疗HER2+阳性乳腺癌。这些药物都是口服的,并且靶向HER2的激酶结构域。
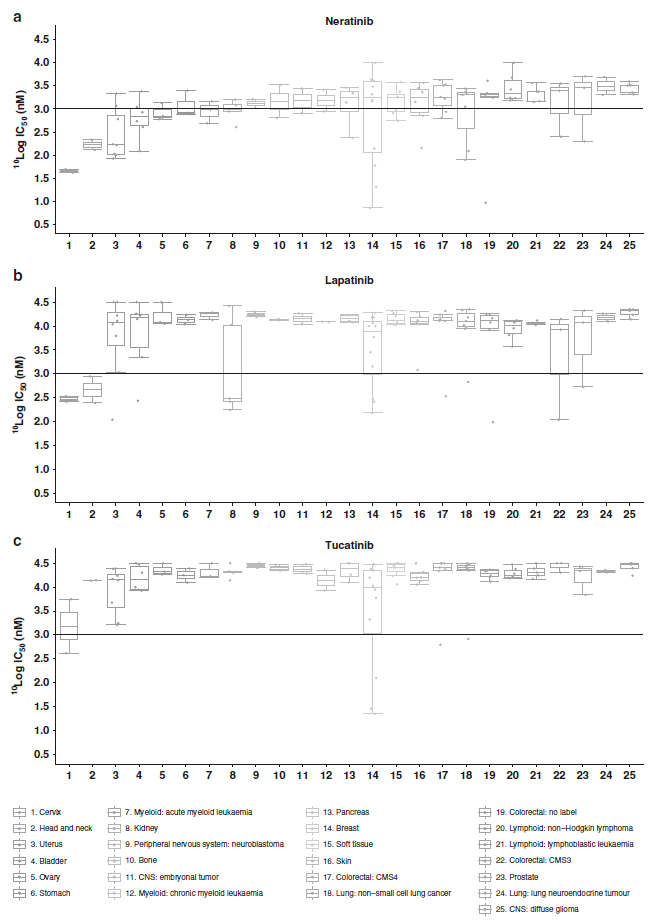
靶向HER2的TKIs的细胞分析
目前关于TKI临床前疗效的直接比较仅限于小规模的研究。随着可用于一线治疗难治性的HER2+乳腺癌的治疗方法的增多,因此急需了解和区分临床认可的相关TKI因素。并通过鉴定新的生物学标志物来定义有益的患者人群。
在该研究中,研究人员共采用了115个癌细胞系直接比较了三种TKI的抗增殖作用。并通过对具有突变、基因拷贝数和表达数据的药物反应谱进行了交叉分析,以鉴定出新的TKI反应/耐药标记。
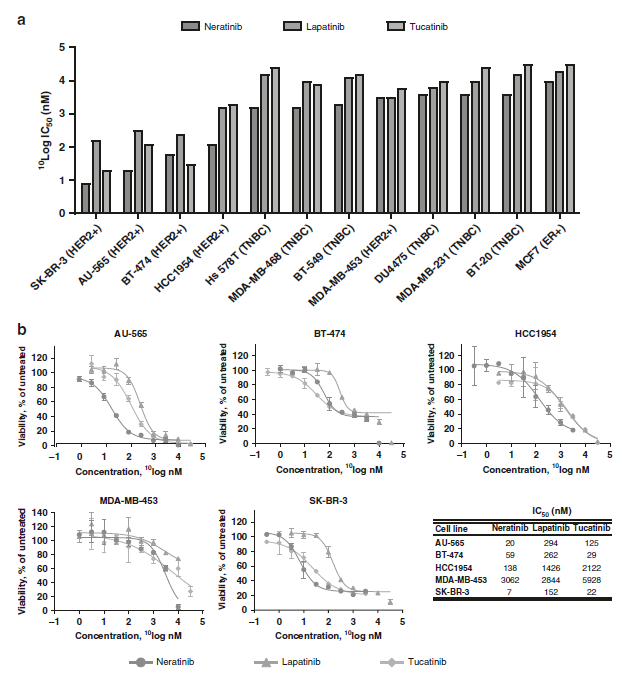
乳腺癌细胞系的给药反应
结果显示,三种TKI对HER2扩增的乳腺癌模型均有效。来那替尼(neratinib)表现出最强的活性,其次是图卡替尼(tucatinib),最后是拉帕替尼(lapatinib)。在HER2突变和EGFR突变的细胞中来那替尼活性最强。进一步的研究显示,HER2、VTCN1、CDK12和RAC1的高表达与三种TKI的反应相关。而DNA损伤修复相关基因的表达与TKI的抗性相关。BRCA2突变与来那替尼和图卡替尼的反应相关,而ATM、BRCA2和BRCA1的高表达则与来那替尼的耐药性相关。
综上,该研究结果显示,来那替尼是HER2扩增、突变和EGFR突变细胞系的最有效的TKI治疗药物。该研究也为靶向HER2的组合疗法的开发提供了相关潜在的耐药机制。
原始出处:
Conlon, N.T., Kooijman, J.J., van Gerwen, S.J.C. et al. Comparative analysis of drug response and gene profiling of HER2-targeted tyrosine kinase inhibitors. Br J Cancer (21 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#比较分析#
95
#抑制剂#
0
#靶向HER2#
86
#酪氨酸激酶#
130
#激酶抑制剂#
121
#激酶#
103