JAMA Oncol:共存突变可影响 EGFR-TKIs的疗效
2018-04-02 肿瘤资讯 肿瘤资讯
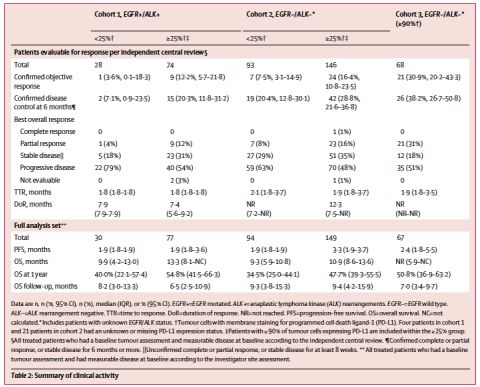
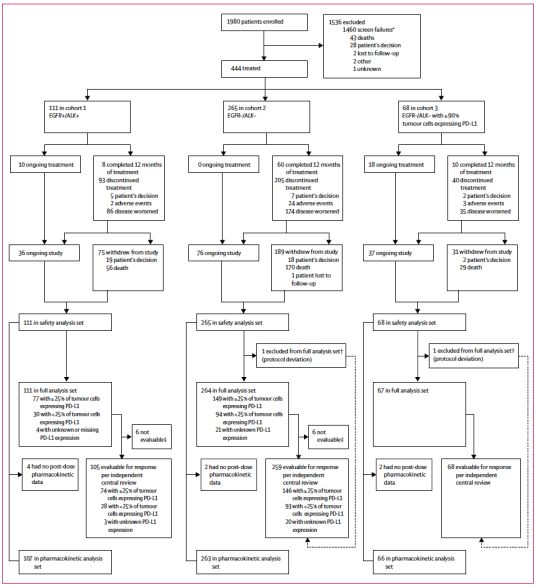
截至目前,已经有10个随机对照III期临床试验证实:对于表皮生长因子受体(EGFR)基因突变的晚期非小细胞肺癌(NSCLC)患者,EGFR-TKIs的疗效显着优于传统化疗。然而对于这些病人,仍有20%~30%出现原发耐药、甚至快速进展,其具体的机制并未完全清楚。来自中山大学肿瘤防治中心的张力教授团队开展了一项队列研究,旨在探讨共存突变(Concomitant mutation)对EGFR-TKIs
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#EGFR-TKIs#
66
#TKIs#
104
#Oncol#
66
#EGFR-TKI#
103
#TKI#
69
#GFR#
89
谢谢梅斯提供这么好的信息,学到很多
116