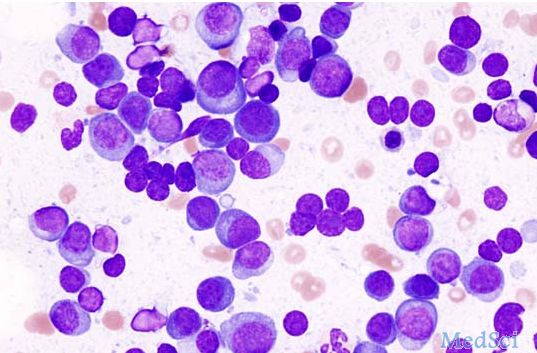
EHA 2016:强生多发性骨髓瘤药物Darzalex+来那度胺+地塞米松三联疗法III期临床显著延长无进展生存期
2016-06-13 佚名 生物谷
美国医药巨头强生(JNJ)近日在第21届欧洲血液学协会(EHA2016)大会上公布了多发性骨髓瘤药物Darzalex(daratumumab)III期MMY3003(POLLEX)临床研究的积极数据。该研究是一项随机、开放标签、多国、多中心、对照III期研究,在569例既往已接受至少一种疗法的多发性骨髓瘤(MM)患者中开展。数据显示,与标准护理方案lenalidomide(来那度胺,一种免疫调节剂
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#I期临床#
57
#多发性#
53
#III#
50
#强生#
71
#生存期#
57
#Darzalex#
80
#无进展生存期#
69
#EHA#
55
#II期临床#
72
#III期#
49