液体活检技术临床应用进展:CTC,ctDNA和外泌体检测
2015-11-07 MedSci MedSci原创
液体活检(Liquid biopsy)的检测方法,可以捕获到进入血液的其它细胞或DNA,从而替代了疾病的诊断,例如肿瘤。关于这些检测方法的价值,现在还有很多不清楚的地方,但是许多医生认为,这些检测方法是一个很大的进步,可能可以为更多的病人实现个体化治疗。 这些检测方法是第一次非介入性地,可重复性地抽取肿瘤样本,医生们从而可以建立基因表达谱,靶向突变用药,快速判断治疗是否有效,及随肿瘤的发
液体活检(Liquid biopsy)的检测方法,可以捕获到进入血液的其它细胞或DNA,从而替代了疾病的诊断,例如肿瘤。关于这些检测方法的价值,现在还有很多不清楚的地方,但是许多医生认为,这些检测方法是一个很大的进步,可能可以为更多的病人实现个体化治疗。
这些检测方法是第一次非介入性地,可重复性地抽取肿瘤样本,医生们从而可以建立基因表达谱,靶向突变用药,快速判断治疗是否有效,及随肿瘤的发展而调节治疗方案。
目前在德州大学MD安德森癌症中心,约10%的有转移性大肠癌的患者正在接受液体活检。
卢煜明教授被誉为无创产前诊断的奠基人。早在1997年,他的研究小组发现孕妇血浆中存在游离的胎儿DNA,也正是这项研究产生了更加安全、简单的唐氏综合症检测方法。卢教授正在与世界各地的实验室竞争开发基于简单血液检测的癌症筛查技术,即液体活检。失活的(dying)癌细胞会释放DNA到血液中,但在癌症早期,癌细胞所释放的DNA量很少,并且会被进入循环系统的健康DNA所掩盖,从而难以检测。卢教授说:“我们的目标非常明确,就是开发一种血液检测,在癌症可治愈之前发现它。”卢教授所在的医院正在进行两项与DNA检测相关的大型研究。其中一项是对1000名乙肝患者进行跟踪,验证DNA检测能够早于超声检测发现肝脏肿瘤。另一项涉及2万人的研究与鼻咽癌相关。这种癌症可能吃咸鱼、遗传易感性以及Epstein-Barr病毒感染有关。卢教授开发的检测方法是希望在人的血浆中检测到失活的癌细胞释放的病毒DNA。卢教授说:“虽然目前通过DNA检测预测患癌的风险成本依然很高,但随着测序技术的不断发展,癌症早期筛查将会变得更加便宜、应用范围更加广泛。之前胎儿检测的费用也很昂贵,但是现在已经降到了800美元,我相信,同样的事情会发生在癌症上。”
液态活检技术之血浆游离循环肿瘤DNA(ctDNA)

血浆游离循环肿瘤DNA (Cell-free Circulating Tumor DNA ,ctDNA)是由肿瘤细胞释放到血浆中的单链或者双链DNA,携带有与原发肿瘤组织相一致的分子遗传学改变。
数十年来,科研人员一直都在寻找能够很好地反映肿瘤情况的生物标志物,与蛋白质类生物标志物相比,循环DNA的表现应该会更好。在临床工作中,蛋白质已经被用来诊断疾病,或者监测治疗效果。但是蛋白类生物标志物检测会出现假阳性结果,因为也有其它原因会导致血液中的蛋白类生物标志物增加。可是ctDNA检测出现假阳性结果的可能性就要低得多,因为我们不是检测ctDNA的水平,而是检测它是否携带有肿瘤特异性的突变,或其它基因组改变信息。
早在1947年Mandel和Metais就发现了循环核酸;30年后Leon等人的研究结果表明肿瘤患者外周血清DNA水平大大高于正常人,之后研究者在肿瘤患者的血浆和血清中检测到了癌基因突变,并且与原发肿瘤相一致。
2013年新英格兰医学杂志The New England Journal of Medicine研究结果发现:ctDNA检测作为一种无创的检测方法,能够真实的反映实体瘤组织中的基因突变图谱与频率,是治疗效果的评估及治疗后临床随访的重要监测指标。
Bettegowda和他的同事最近报道了一篇文章,称ctDNA水平在早期和晚期肿瘤(各种癌症)中存在差异。研究人员发现,在640例患者中,ctDNA可检测超过75%的晚期胰腺癌,卵巢癌、结直肠癌、膀胱癌、胃癌、乳腺癌、黑色素瘤、肝癌,以及头颈癌。然而,在原发性脑、肾、前列腺癌和甲状腺癌的检测却不到50%。此外,在206例转移性结直肠癌患者中,源自KRAS基因突变的ctDNA具有87.2%的敏感性和99.2%的异质性。研究人员还发现,96%的表皮生长因子受体被抑制后复发的患者体内有ctDNA,这就表明在丝裂原活化蛋白激酶途径中发生了单基因或多基因突变。
ctDNA作为一种新的肿瘤标志物,将在肿瘤的诊断、治疗及预后检测等方面发挥重要作用,尤其对于一些不具有典型临床症状、检查无特异性和诊断困难的肿瘤可避免复杂的、具有创伤性的活检。ctDNA来自肿瘤细胞的体细胞突变,不同于遗传突变的是,遗传突变存在于体内每个细胞。因此,ctDNA是一种特征性的肿瘤生物标记物,并且还可以被定性、定量和追踪。
ctDNA临床应用领域

适用范围:实体瘤患者
随着肿瘤分子生物学研究的进展,血浆游离循环肿瘤DNA检测技术必将成为临床肿瘤早期诊断、预后判断、跟踪随访等的一项重要的分子生物学检测手段。
液态活检技术之循环肿瘤细胞(CTC)监测技术
循环肿瘤细胞 (Circulating tumor cell, CTC) 是指从实体瘤中脱离出来并进入外周血液循环的肿瘤细胞。
早在1889年,Paget提出了“种子和土壤”的学说,强调癌细胞和微环境之间的关系,认为肿瘤转移的形成,是处于旺盛生长状态的肿瘤细胞作为“种子”,当遇到合适的器官、组织的基质环境,即“土壤”时,就会发生肿瘤的转移。期间,有专家提出了“解剖——机械”学说,认为CTC的转移为随机现象,CTC在最先到达脏器的毛细血管或淋巴结发生机械性滞留。在1896年,澳大利亚学者Ashworth在一例转移性肿瘤患者血液中首次观察到从实体肿瘤中脱离并进入血液循环的肿瘤细胞,并率先提出了CTC的概念。从上世纪末以来CTC检测技术得到了不断的改进,随之带来的是CTC检测在临床的应用。
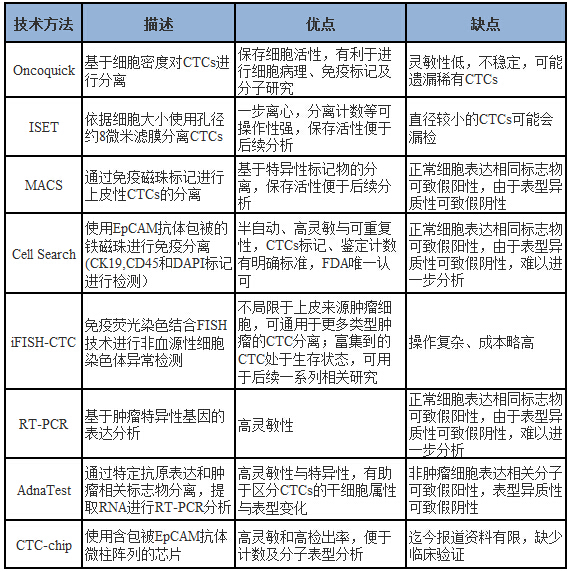
随着CTC临床应用价值凸显,许多研究机构和研发团队都在推出不同的CTC检测技术。目前,CTC检测技术主要分为以下几种:
已经完成及正在进行的大量研究显示,CTC在临床上具有很大的应用价值。目前,CTC在临床上的应用主要包括以下几个方面:
1.早期筛查
研究发现,在早期肿瘤患者中,利用影像学还未发现病灶时已经可以在外周血中检测到CTC,因此CTC可以用于肿瘤的早期诊断,2007年ASCO就将CTC纳入了肿瘤标志物。在临床上,也遇到过非常典型的案例,一受检者利用CTC做肿瘤早期筛查,在外周血中检出1个CTC,后又通过数字PCR技术对ctDNA进行了定量分析,结果提示该患者肿瘤与结直肠相关性较大。在随后进行的肠镜检查中,在受检者结直肠部位发现一个低分化腺瘤。
2.快速疗效评估——作为肿瘤生物动力学标志物
通过CTC在不同治疗阶段的数目变化,可辅助快速评估手术、放化疗及其他治疗手段的疗效。
3. 辅助肿瘤患者分期分级
通过检测CTC数目,辅助评估肿瘤患者的分期及分级。血液系统是肿瘤转移的重要途径,是否发生远处转移是判断临床分期的标准之一。近年来,CTC检测在临床上的应用使之成为了TNM传统分期系统的有效补充,从而指导下一步的治疗。
4. 判断患者是否需要辅助化疗
术后CTC数目大于阈值,建议强化术后辅助化疗;CTC数目小于阈值,建议采用标准辅助化疗。
5. 监测癌症转移复发风险
CTC数目上升,提示肿瘤进展,转移复发风险增大;CTC数目下降,提示肿瘤缓解,转移复发风险降低。
6. 提供预后相关的分子生物学特征
目前研究已经证实血液中检测到的CTC可以作为乳腺癌、前列腺癌和结肠癌等肿瘤的独立预后因素。CTC监测数目越高,提示患者预后较差。在转移性乳腺癌患者接受系统治疗之前,每7.5 ml血液中CTC计数超过5 个, 提示更短的无进展生存时间和总生存时间。在转移性结肠癌患者中,每7.5 ml血液中CTC计数超过3个,患者中位总存活期和无进展存活期都明显缩短。
7. 监测耐药情况——基于获得连续样本的便利性
通过检测CTC数目变化,实时监测肿瘤药物耐药性的发生。
CTC在肿瘤诊断、治疗和监控等方面的临床表现已逐渐崭露头角,是目前最具发展潜力的肿瘤无创诊断和实时疗效监测手段,临床应用价值极其显著。
虽然实体肿瘤的检测仍然是癌症诊断中的常规程序,但新一代测序等现代技术,已经使科学家们能够更详细地跟踪肿瘤的组织起源。许多肿瘤会脱落细胞,称为外泌体(exosome)的囊泡,也有DNA进入血液和其他体液的痕迹。最近的研究表明,这些碎片可以作为标记物,来监测疾病的进展,甚至有助于研究人员在症状出现之前诊断癌症。
结果发现,肿瘤DNA通常可在血液样本中检测到。例如,6月5日在《JAMA Oncology》发表的一项研究中,研究人员检测了4000多名孕妇的血液样本——为了确定胎儿中的染色体异常而抽取的,确定了三例孕产妇癌症:一例卵巢癌,一例滤泡性淋巴瘤,和一例霍奇金淋巴瘤。本文共同作者、鲁汶大学人类遗传学中心的Joris Vermeesch说:“我们发现,在大多数的这些肿瘤中,即使是低等级的肿瘤,也可以用一个人的血液,用于研究肿瘤生物学。”
这样的“液体活检”不仅仅是血液和血浆样品。在其他研究中,研究人员将膀胱癌患者术后复发风险,与尿液中的DNA甲基化水平关联起来,检测粪便样本中的肠癌DNA,并鉴定了头颈部癌患者唾液中的癌症相关突变。以前,这种分子测试被用来监测晚期疾病和肿瘤转移。现在,随着越来越多的精确工具,即使在疾病的最早期阶段,也可以在血液中发现少量的癌细胞和DNA。
约翰霍普金斯大学医学院的Bert Vogelstein称:“粪便和尿液可以检测结直肠癌或膀胱癌,但血液能够检测所有的癌症——至少从概念上来说。然而,从逻辑上说,检测非常少量的DNA一直都存在挑战。”
共同证据
去年,在《Science Translational Medicine》发表的一项包括640例患者的研究中,研究人员报道称,可以在大约40%至70%的几种癌症中检测到循环肿瘤DNA,包括脑瘤、前列腺癌和卵巢癌。例如,在晚期结直肠癌患者中,循环肿瘤DNA可被用来确定87%的病例中的KRAS基因突变。
完整的癌细胞也可以进入血液循环。早期有研究尝试依靠识别表面抗原或其他标记,捕捉这些循环肿瘤细胞(CTCs)。但是,根据肿瘤的类型、病期和其他因素,CTCs可能带着不同的分子面具。然而,今年早些时候,哈佛医学院的Mehmet Toner及其同事在《Nature Methods》发表论文指出,微流体装置可以用“不依赖全血肿瘤特异性标记”的物理方法,捕获这些细胞。Toner告诉The Scientist杂志说:“完整的细胞有着巨大的价值。你可以研究DNA、RNA、信号分子、磷酸化模式、表观遗传学——这比一个单一的生物标志物更加丰富。从长远来看,我们可以培养这些细胞,来测试药物的敏感性,真正走向个性化医学。”
除了DNA和全细胞之外,最近的研究表明,肿瘤细胞脱落的外泌体,也可作为替代的癌症生物标志物。6月24日,德克萨斯大学MD安德森癌症中心研究人员带领的一个研究小组,在《Nature》发表论文,描述了外泌体的一种血清检测法——它携带着DNA、RNA和蛋白质,可以用来成功区分患者早期、晚期胰腺癌与良性胰腺疾病或健康受试者。
但循环肿瘤痕迹的罕见性——无论DNA、整个CTCS还是脱落的囊泡,迄今为止都具有临床应用的挑战。根据Vogelstein介绍,提高这种分子测试的灵敏度和特异性,对于建立其临床效用是至关重要的。除了消除假阳性,这些结果对于了解“为什么有些肿瘤不能在血液和其他液体中被跟踪到”,也是必不可少的。
Vogelstein说:“目前,我们不知道局限是技术性的还是生物学的。我们发现,40%到70%之间的肿瘤,是可检测的。但是,如果其余的早期癌症不分泌单一分子的循环肿瘤DNA,那么无论我们的技术有多好,它都不重要。”
大部分的生物学基础还不清楚,伦敦大学学院的Tim Forshew通过电子邮件告诉The Scientist杂志:“我们还不完全知道循环肿瘤基因是如何进入血液循环的,以及根据不同类型的癌症它们有何不同。我们也不完全了解是什么影响着它迅速从血液中清除。”
尽管如此,使用一种简单的血液测试来诊断癌症,并指导治疗策略的可能性,已经鼓舞着一些公司,他们现在正在竞相研制检测方法。
早期应用
Forshew说:“循环肿瘤标志物的商业利益是巨大的。”他在Inivata(提供循环肿瘤DNA为基础的诊断测试的几个公司之一)带领技术研发。在Forshew的心里,这种技术最重要的应用是,研究癌症的遗传学,而不是轻易操作的活检。
其他几家公司——包括Epic Sciences、Johnson & Johnson’s Janssen Diagnostics、SRI International和Guardant,目前提供循环肿瘤DNA和细胞的测试。然而,这些测试的临床应用迄今已被局限在监测肿瘤转移,在较小程度上,也监测治疗反应。
从事临床研究的科学家正在努力将血液中的肿瘤DNA与特定的疾病参数关联起来,如手术切除肿瘤后的复发风险。Vogelstein说:“这不同于预测预后结果,这实际上是检测尚未出现临床或影像学迹象的神秘疾病,这样我们就可以及早地实施治疗。”
与Vogelstein合作,澳大利亚Walter and Eliza Hall医学研究所的Jeanne Tie和她的同事,采用循环肿瘤DNA,来评估哪些患者最有可能受益于II期大肠癌手术后的化疗。一般情况下,一大部分患者在手术后接受辅助化疗。但只有4%到5%的患者似乎从中受益。其余的患者,要么手术证明是充分的,要么尽管化疗还是出现了癌症复发。该小组的初步结果,提交到去年的美国临床肿瘤学会会议,表明复发风险与循环肿瘤DNA水平密切相关。研究人员正在计划一项更大的随机试验,来评估循环肿瘤DNA指示化疗实施的效用。Tie说:“通过使用血液测试来指导化疗,我们不仅可以提高生存率,而且还可以减少接受不必要化疗的患者数量。”
与以前使用的测量(如前列腺特异性抗原,甚至是由健康细胞释放的)相比,肿瘤DNA、CTCs与肿瘤来源的外泌体,都是“更高价值”的标志物。他说:“这些新的标志物,提供了一个惊人的机会来管理癌症。以前,我们总是落后于疾病一步。有了这些更具体、更敏感的工具,我们终于可以向前迈进一步。”
相关文献
Amant F, Verheecke M, Wlodarska I, Dehaspe L, Brady P, Brison N, Van Den Bogaert K, Dierickx D, Vandecaveye V, Tousseyn T, Moerman P, Vanderstichele A, Vergote I, Neven P, Berteloot P, Putseys K, Danneels L, Vandenberghe P, Legius E, Vermeesch JR.Presymptomatic Identification of Cancers in Pregnant Women During Noninvasive Prenatal Testing.JAMA Oncol. 2015 Sep 1;1(6):814-9
Ma M, Zhu H, Zhang C, Sun X, Gao X, Chen G."Liquid biopsy"-ctDNA detection with great potential and challenges. Ann Transl Med. 2015 Sep;3(16):235
Ignatiadis M, Lee M, Jeffrey SS.Circulating Tumor Cells and Circulating Tumor DNA: Challenges and Opportunities on the Path to Clinical Utility. Clin Cancer Res. 2015 Nov 1;21(21):4786-800
Gray ES, Rizos H, Reid AL, Boyd SC, Pereira MR, Lo J, Tembe V, Freeman J, Lee JH, Scolyer RA, Siew K, Lomma C, Cooper A, Khattak MA, Meniawy TM, Long GV, Carlino MS, Millward M, Ziman M.Circulating tumor DNA to monitor treatment response and detect acquired resistance in patients with metastatic melanoma.Oncotarget. 2015 Sep 22. doi: 10.18632/oncotarget.5788
Wang Y, Springer S, Zhang M, McMahon KW, Kinde I, Dobbyn L, Ptak J, Brem H, Chaichana K, Gallia GL, Gokaslan ZL, Groves ML, Jallo GI, Lim M, Olivi A, Quinones-Hinojosa A, Rigamonti D, Riggins GJ, Sciubba DM, Weingart JD, Wolinsky JP, Ye X, Oba-Shinjo SM, Marie SK, Holdhoff M, Agrawal N, Diaz LA Jr, Papadopoulos N, Kinzler KW, Vogelstein B, Bettegowda C.Detection of tumor-derived DNA in cerebrospinal fluid of patients with primary tumors of the brain and spinal cord.Proc Natl Acad Sci U S A. 2015 Aug 4;112(31):9704-9.
Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, Bartlett BR, Wang H, Luber B, Alani RM, Antonarakis ES, Azad NS, Bardelli A, Brem H, Cameron JL, Lee CC, Fecher LA, Gallia GL, Gibbs P, Le D, Giuntoli RL, Goggins M, Hogarty MD, Holdhoff M, Hong SM, Jiao Y, Juhl HH, Kim JJ, Siravegna G, Laheru DA, Lauricella C, Lim M, Lipson EJ, Marie SK, Netto GJ, Oliner KS, Olivi A, Olsson L, Riggins GJ, Sartore-Bianchi A, Schmidt K, Shih lM, Oba-Shinjo SM, Siena S, Theodorescu D, Tie J, Harkins TT, Veronese S, Wang TL, Weingart JD, Wolfgang CL, Wood LD, Xing D, Hruban RH, Wu J, Allen PJ, Schmidt CM, Choti MA, Velculescu VE, Kinzler KW, Vogelstein B, Papadopoulos N, Diaz LA Jr.Detection of circulating tumor DNA in early- and late-stage human malignancies.Sci Transl Med. 2014 Feb 19;6(224):224ra24
Romero D.Breast cancer: Tracking ctDNA to evaluate relapse risk.Nat Rev Clin Oncol. 2015 Nov;12(11):624.
Gold B, Cankovic M, Furtado LV, Meier F, Gocke CD.Do Circulating Tumor Cells, Exosomes, and Circulating Tumor Nucleic Acids Have Clinical Utility?: A Report of the Association for Molecular Pathology. J Mol Diagn. 2015 Apr 8. pii: S1525-1578(15)00047-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










太厉害了,完善了现有的肿瘤检测系统,对下一步的治疗指导也很有用!
129
#临床应用#
62
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
117
#应用进展#
69
#CTC#
69
#液体活检技术#
67
#活检#
77
#体检#
93
系统综述
126
非常好
160