厄洛替尼对EGFR突变的IA-IIIA期NSCLC术后维持治疗可能获益(SELECT研究)
2014-06-15 钟文昭 吴一龙 中国医学论坛报
表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKI)治疗EGFR敏感突变的晚期非小细胞肺癌(NSCLC)疗效卓越,多个随机对照研究确定了一线使用EGFR-TKI可改善EGFR突变肺癌的肿瘤缓解率和无进展生存期(PFS),本届ASCO上,报告了LUX3和LUX6研究的汇总结果,一线TKI可改善EGFR突变肺癌,尤其是19缺失肺癌的总体生存(OS)。EGFR突变肺癌TKI的适应症已从二线到一线,能否从
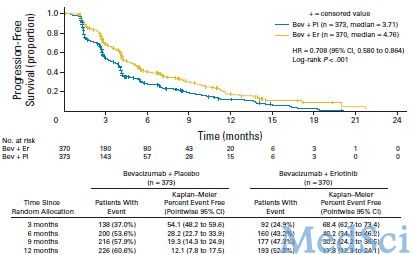
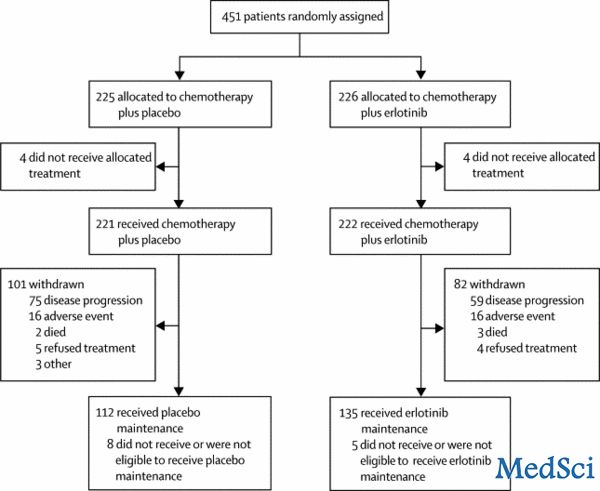
表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKI)治疗EGFR敏感突变的晚期非小细胞肺癌(NSCLC)疗效卓越,多个随机对照研究确定了一线使用EGFR-TKI可改善EGFR突变肺癌的肿瘤缓解率和无进展生存期(PFS),本届ASCO上,报告了LUX3和LUX6研究的汇总结果,一线TKI可改善EGFR突变肺癌,尤其是19缺失肺癌的总体生存(OS)。EGFR突变肺癌TKI的适应症已从二线到一线,能否从进展期一线进一步扩展到早中期肺癌辅助治疗,从延长晚期肺癌PFS到提高手术患者的治愈率是一个备受关注的研究方向。TKI临床应用近十年,虽然目前ESMO指南明确反对辅助TKI,NICE指南则提示可作为研究的方向,然而多达51%受访医师仍建议辅助靶向治疗。系列临床研究为此孜孜不倦的探索,直至今天对于TKI辅助治疗时程、疗效、获益人群等规律仍然颇具争议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了,谢谢作者分享!
104
#III#
60
#SeLECT#
81
#厄洛替尼#
62
#GFR#
57