ECC 2015:奥曲肽联合177Lu—DOTATATE对神经内分泌肿瘤可能有效(NETTER-1研究)
2015-10-01 MedSci MedSci原创
9月26日12:30,在ECC2015召开的第二次新闻发布会上,又有两项重要的最新研究摘要(LateBreakingAbstract)——RADIANT-4和NETTER-1研究亮相。在此对NETTER-1研究作一简介。 NETTER-1研究的主要研究者、同样来自美国的Philippe Ruszniewski教授指出,NET是
9月26日12:30,在ECC2015召开的第二次新闻发布会上,又有两项重要的最新研究摘要(LateBreakingAbstract)——RADIANT-4和NETTER-1研究亮相。在此对NETTER-1研究作一简介。

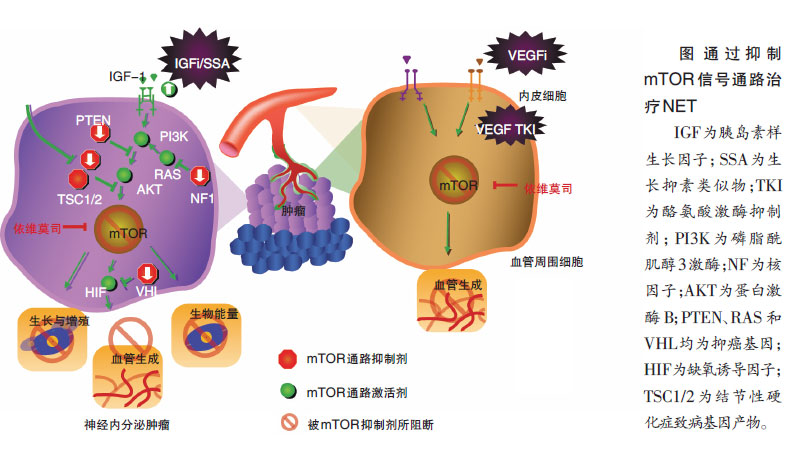
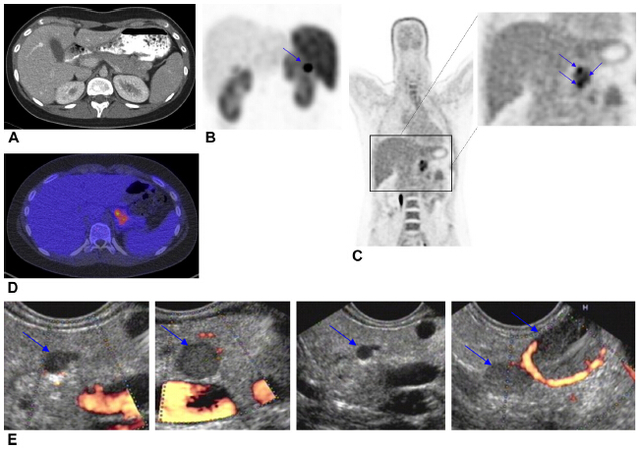
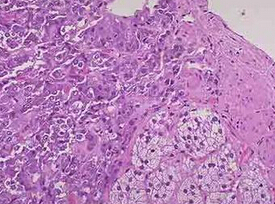
NETTER-1研究的主要研究者、同样来自美国的Philippe Ruszniewski教授指出,NET是一种起源于不同器官神经内分泌细胞的一组疾病。虽然NET较为罕见,但其却是胃肠道恶性肿瘤中第二常见的肿瘤,且近年来的发病率有增长。目前对一线生长抑素类似物治疗进展后的晚期中肠NET,治疗药物很有限,而肽受体放射治疗(PRRT)177Lu—DOTATATE靶向生长激素抑制素受体,Ⅲ期NETTER-1研究就探讨了177Lu—DOTATATE在上述患者中的应用价值。
研究共纳入229例患者,随机接受生长激素抑制素奥曲肽联合177Lu—DOTATATE治疗或单纯生长激素抑制素octreotideLAR。结果显示,前者的中位无进展生存(PFS)还未达到,后者的PFS期为8.4个月。目前的结果表明接受177Lu—DOTATATE治疗有额外的PFS获益。177Lu—DOTATATE组的客观缓解率(ORR)达到19%,而奥曲肽组为3%(P<0.0004),中期分析的总生存(OS)也显示前者有延长趋势。Ruszniewski教授认为,鉴于在经治晚期中肠NET的有效治疗选择有限,该项Ⅲ期研究中的阳性结果使177Lu—DOTATATE成为了重要进展,该结果有望影响临床实践。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#奥曲肽#
66
#TTE#
0
#分泌#
0
#内分泌肿瘤#
60
#神经内分泌#
47
#ECC#
48
#NET#
51
#ATA#
50