JACC:CORONOR研究:稳定冠心病患者再次心梗率0.8%
2017-05-02 许菁 中国循环杂志
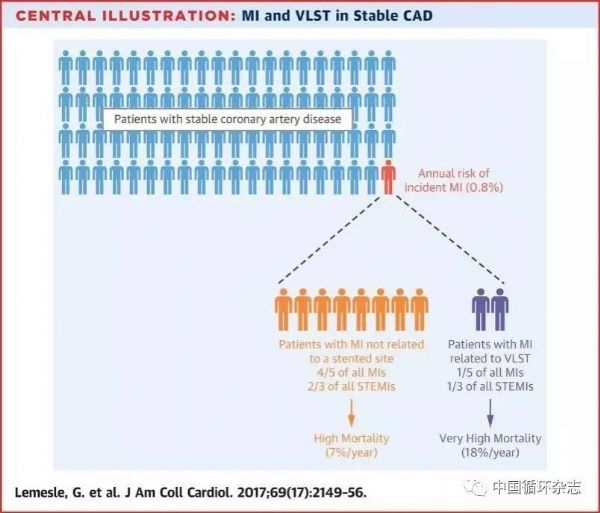
近期,JACC发表的CORONOR研究数据显示,稳定型冠心病患者的再次心梗年发生率为0.8%。ST段抬高型心肌梗死占1/3。1/5再次心梗的发生源于晚期支架内血栓形成。再次心梗使患者死亡风险增加1倍,年死亡率达7%。研究者发现,心血管病危险因素控制不佳如当前吸烟,高脂血症、糖尿病以及多支病变、持续心绞痛均增加再次心梗发生风险。而之前做过搭桥手术降低心梗再发风险。另外,对于接受过PCI的患者,晚期支
近期,JACC发表的CORONOR研究数据显示,稳定型冠心病患者的再次心梗年发生率为0.8%。ST段抬高型心肌梗死占1/3。1/5再次心梗的发生源于晚期支架内血栓形成。再次心梗使患者死亡风险增加1倍,年死亡率达7%。
另外,对于接受过PCI的患者,晚期支架内血栓导致的再次心梗多为ST段抬高型心肌梗死。晚期支架内血栓使死亡率增加4倍,年死亡率达18%。
研究者对4094例稳定型冠心病患者随访5年。
原始出处:
Gilles Lemesle, Olivier Tricot, Thibaud Meurice, et al. Incident Myocardial Infarction and Very Late Stent Thrombosis in Outpatients With Stable Coronary Artery Disease. J Am Coll Cardiol. 2017 May 2.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JACC#
46
#CORONOR研究#
46
学习了,感谢分享!
79
涨知识,学习了
0
#ACC#
53
#冠心病患者#
49
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。点赞啦!
87
非常好的文章,学习了,很受益
82
学习一下知识,谢谢
88