早发和晚发性结直肠癌风险增高更多是饮酒的“锅”还是基因的错?《柳叶刀》子刊最新研究:风险最多可增加近3倍!
2022-05-28 LILYMED MedSci原创
eClinicalMedicine:饮酒、多基因风险评分以及早发和晚发性结直肠癌风险
尽管≥50岁成年人的结直肠癌(CRC)发病率显着下降,但许多国家,特别是高收入国家,现在正在经历早发性CRC(EOCRC)发病率的增加。有证据表明,EOCRC 和晚发性 CRC (LOCRC) 具有明显的环境和遗传危险因素以及临床病理学特征。
过量饮酒是CRC的既定危险因素之一,并且还被认为增加EOCRC风险。几项研究检查了在全基因组关联研究(GWAS)中鉴定的CRC相关单核苷酸多态性(SNP)与CRC风险环境风险因素的相互作用,但基因-环境相互作用的证据仍然有限。相关研究往往受到单一遗传变异和有限功率的微弱影响,特别是考虑到需要对多种测试进行调整。对于环境因素与综合遗传指标(例如基于多个疾病相关位点的多基因风险评分(PRS))的相互作用的分析,统计能力可能要高得多。然而,缺乏证据证明酒精摄入与CRC风险(总体和诊断时的年龄)在PRS水平上的潜在差异相关性。不过,这些证据对于加强风险分层和有针对性的预防工作可能具有高度相关性。此外,将减少饮酒的影响与预定遗传风险的影响进行比较可能是有用的,这可能有助于有效的风险沟通。

因此,本研究的目的是全面评估不同水平PRS下饮酒与整体CRC风险,EOCRC风险和LOCRC风险的关联,并使用最近开发的指标“遗传风险当量(GRE)”量化饮酒的影响,这可能有助于比较环境和遗传因素的风险。

本研究使用多元逻辑回归评估酒精消费与结直肠癌(CRC)在PRS水平上的关联,基于来自一项基于人群的大型病例对照研究的5104个CRC病例和4131个对照组的140个CRC相关位点。我们使用“遗传风险当量(GRE)”比较了酒精消费和PRS对CRC风险的影响,并对早发性CRC(EOCRC,<55年)和晚发性CRC(LOCRC,≥55年)进行了具体分析。
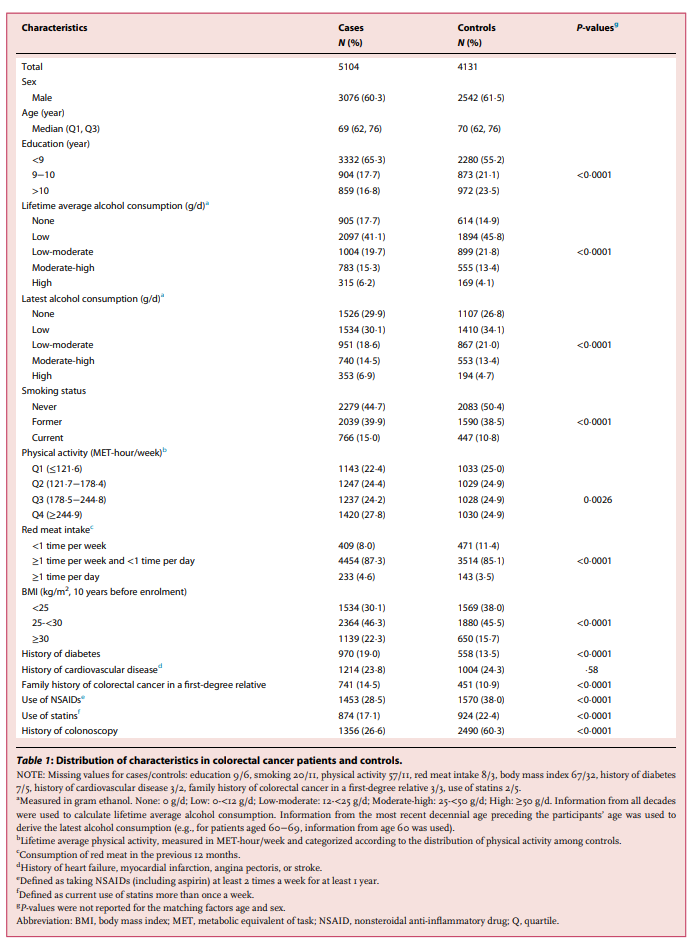
研究人群特征
表 1 总结参与者特征。60.3%的病例和61.5%的对照组为男性,中位年龄分别为69岁和70岁。与对照组相比,这些病例更多是受教育程度较低,酗酒、戒酒或目前吸烟,超重或肥胖,一级亲属有糖尿病史或CRC家族史。他们很少使用非甾体抗炎药或他汀类药物,也很少做结肠镜检查。病例的基线特征也因诊断年龄而异(<55/≥55岁)。
 饮酒和多基因风险评分与CRC总体风险的关系
饮酒和多基因风险评分与CRC总体风险的关系
由于具有CRC风险的不同酒精消费类别的OR不因性别而异(终生和新晋饮酒与性别相互作用的P值分别为0.57和0.055,补充表S7),研究人员在以下分析中合并了两种性别。经过多种协变量调整后,与终生低饮酒相比,终身不饮酒、中高和高饮酒量与结直肠癌风险显著增加16%、22%和51%相关 (表2)。新进饮酒与结直肠癌风险的相关性也非常相似。酒精消费(分类/连续)与PRS水平之间的相互作用没有达到统计学意义。酒精摄入与CRC风险之间存在j型剂量-反应关系。
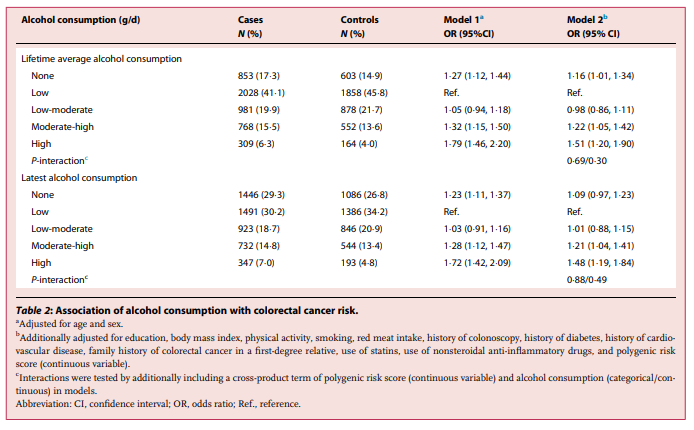
酒精摄入与CRC风险之间的剂量-反应关系在低PRS和高PRS参与者中相似。与低 PRS 组终生低酒精摄入组相比,高 PRS 组终生戒酒、低、低、中、高饮酒量组的CRC风险分别增加了2.1倍、1.7倍、1.8倍、2.2倍和2.6倍。同样,新近酒精摄入也有类似的联系。至于PRS对CRC风险的个体影响,与低PRS水平相比,高PRS与CRC,EOCRC或LOCRC的风险增加1.9倍显着相关。
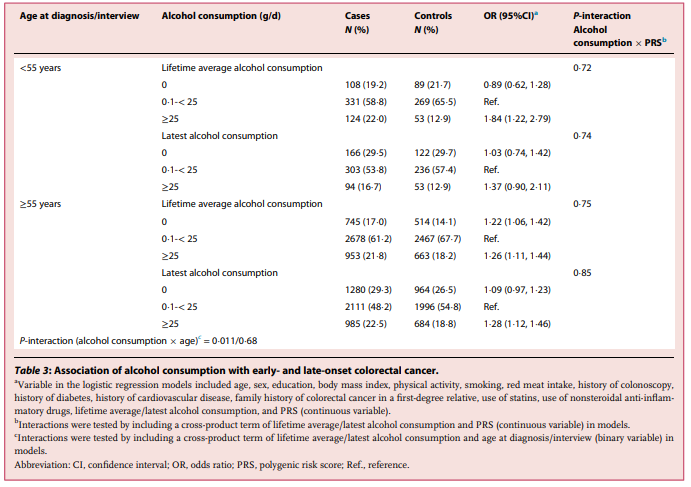
饮酒和多基因风险评分与EOCRC和LOCRC的关联
研究人员观察到终生平均饮酒量与年龄CRC风险之间的关联存在显着差异(表3)。一生平均饮酒≥25 g/d与EOCRC风险增加1.8倍(95% CI 1.2-2.8)相关,强于LOCRC风险(OR 1.3,95% CI 1.1 – 1.4)(CRC风险与年龄交互作用的p值=0.011,错误发现率调整后p值=0.066),但没有观察到新近饮酒的差异相关性。饮酒和PRS在EOCRC或LOCRC风险方面的相互作用同样没有达到统计学意义。当以50岁为截止年份时,饮酒与EOCRC风险之间的相关性也更强,尽管饮酒与年龄在CRC风险上的相互作用没有达到统计学意义(与年龄相互作用的p值分别为0.18和0.43,终生或新近饮酒)。研究人员同样发现同样发现PRS和饮酒对EOCRC风险(<50年)和LOCRC风险(≥50年)的独立贡献。
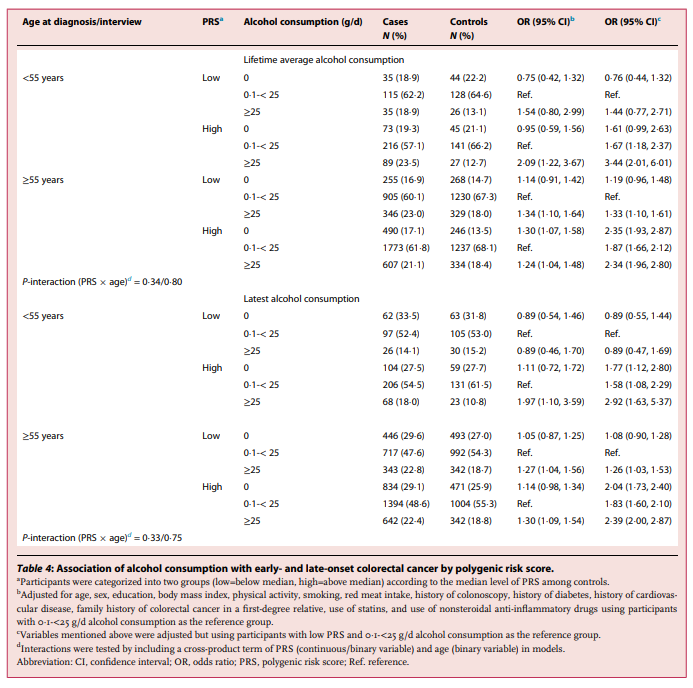
PRS与EOCRC和LOCRC均独立相关,在高PRS的重度饮酒者中风险最高(表4)。与低 PRS 和低饮酒量(0.1-<25 g/d)的受试者相比,PRS 高且终生大量饮酒(≥25 g/d)的患者发生 EOCRC 的风险增加了 3.4 倍(95% CI 2.0–6.0),但 LOCRC 的风险增加了 2.3 倍(95% CI 2.0–2.8)。在新近酒精消费中观察到类似的模式。
按酒类型、癌症部位和癌症分期进行亚组分析
与对照(纯乙醇:0.1-7 g/d)相比,长期喝葡萄酒、啤酒和烈性酒与CRC风险分别显著升高21%、23%和11%。与同一对照相比,啤酒和白酒的终生高平均饮酒量(纯乙醇:>7 g/d)分别与CRC风险增加21%和50%显著相关,但中高酒精摄入葡萄酒风险没有增加。在新近酒精消费中观察到类似的模式。在CRC位置和分期的关联分析中,终生高饮酒量(纯乙醇:≥25 g/d)与远端CRC风险(OR 1.38,95% CI 1.20–1.59)的关联似乎比近端结肠癌风险(OR 1.14,95% CI 0.96–1.35, P-异质性=0.015)更明显。据癌症分期,高酒精消费量和结直肠癌风险之间没有显著的统计学差异。
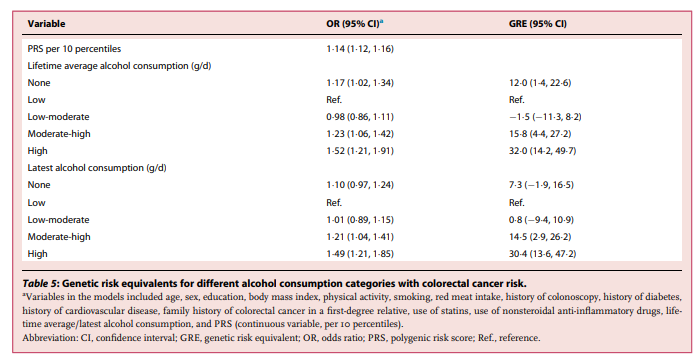
不同酒精消费类别的GREs估算
终生高饮酒对CRC风险的估计影响相当于PRS水平升高32(GRE 32,95%CI 14-50)百分位数的影响(表5)。EOCRC的终生平均饮酒量≥25 g / d的GRE特别高(GRE 47,95%CI 12-82),而对于LOCRC(GRE 18,95%CI 8-29)则不太明显(图1)。与终生平均酒类消费量低的参与者相比,终生平均酒类(>7 g / d)的参与者的GRE最高,为31(95%CI 1-61)。终生平均啤酒量(7 g/d)的GRE值为15 (95% CI 4-25)。此外,终生平均饮酒量≥25 g/d的远端CRC风险GRE为23(95% CI 13-33),高于近端结直肠癌风险GRE(GRE 11,95% CI −4 25)。
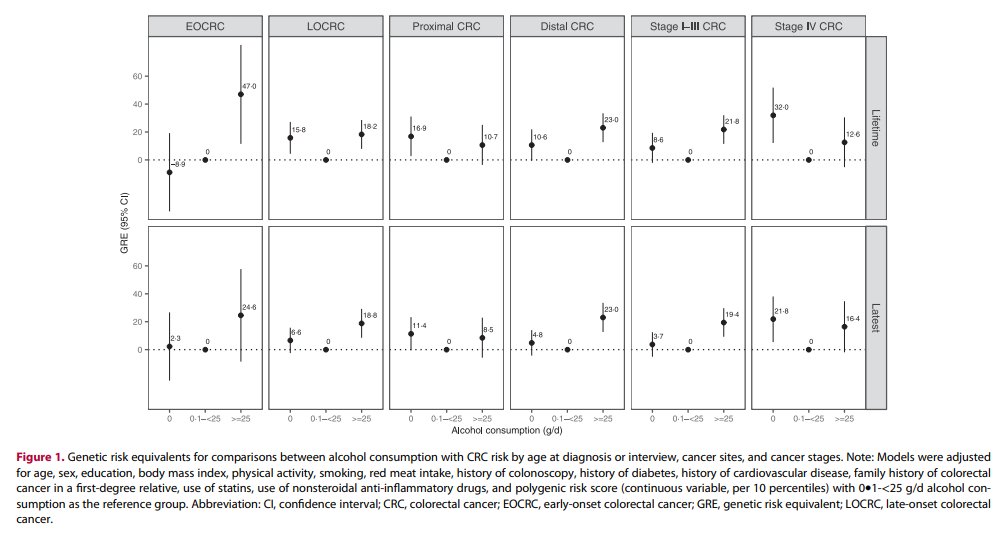
在这项基于人群的大型研究中,过量饮酒以及较低程度的戒酒与CRC风险增加有关。长期大量饮用啤酒和烈性酒而非葡萄酒与CRC风险增加显著相关。重度饮酒与结直肠癌风险的相关性在EOCRC比LOCRC更强,远端 CRC 的相关性比近端 CRC 更显著。酒精消费与PRS水平与CRC风险之间的独立关系,通过共同考虑,可以更有效地进行风险鉴别,特别是对于EOCRC风险。此外,GRE的估计值表明,避免大量饮酒对CRC风险的影响可能相当于大大降低了预先确定的多基因风险。
原文来源:
Xuechen Chen, et al. Alcohol consumption, polygenic risk score, and early- and late-onset colorectal cancer risk. eClinicalMedicine 2022;49: 101460 Published online xxx https://doi.org/10.1016/j. eclinm.2022.101460
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#结直肠癌风险#
98
#早发#
84
#最新#
88
#癌风险#
98
#结直肠#
82
#增高#
93
#增高#
90