PLoS One:缺血性卒中后要早点坐起来?
2016-04-10 MedSci MedSci原创
背景:长时间制动与住院期间并发症的发生相关。然而,没有明确的指南推荐缺血性中风患者早期运动是可行的。目的:由于已证明早期运动是可行的和安全的,研究者假设,早期坐起来可能对卒中患者的预后是有益的。方法:这项多中心前瞻性研究以随机对照的方式,检测缺血性卒中急性期患者两种不同坐的方式。纳入标准为,患者年龄18岁以上,无大面积脑梗死或任何坐的禁忌症。在早期坐起来组,患者尽可能早的离开床坐起来,但是不能迟于
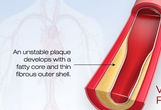
背景:长时间制动与住院期间并发症的发生相关。然而,没有明确的指南推荐缺血性中风患者早期运动是可行的。
目的:由于已证明早期运动是可行的和安全的,研究者假设,早期坐起来可能对卒中患者的预后是有益的。
方法:这项多中心前瞻性研究以随机对照的方式,检测缺血性卒中急性期患者两种不同坐的方式。纳入标准为,患者年龄18岁以上,无大面积脑梗死或任何坐的禁忌症。在早期坐起来组,患者尽可能早的离开床坐起来,但是不能迟于卒中后1天;然而,延迟离开床坐起来组,首次坐起来在卒中后3天。主要预后为卒中后3个月mRS(0-2)。次要预后为:a)医疗并发症,b)住院天数和c)对手术的耐受性。
结果:研究共有167名患者,随机化后排除29例。138例患者中,63例在早期坐起来组,75例在延迟坐起来组。两组间,卒中患者的主要预后没有差异,3个月mRS评分为0-2的比率分别为76.2%,77.3%。两组间次要预后也无明显差异,并且在实验过程中,两组耐受性良好。
结论:由于入组患者较慢,分析的数据比预期的少。结果是,研究者只能检测到早期坐起来的有益的/有害的影响为+ / - 15%,并且效力为37%。然而,研究数据足以排除高于25%的效应值,效力为80%,显示早期坐起来不可能对卒中预后有直接的影响。另外,研究者不能对主要预后进行双盲评估。考虑到这些不足,研究结果可能有助于指导指定更有效地卒中康复措施,并且指导设计未来的急性卒中试验,涉及床上的活动或者,其他运动方案。
原文出处:
Herisson F, Godard S, Early Sitting in Ischemic Stroke Patients (SEVEL): A Randomized Controlled Trial. PLoS One. 2016 Mar 29
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#缺血性卒#
81
#卒中后#
73
#缺血性#
75
#Plos one#
60
文章值得学习
147
不错不错
109