Nat Med:肿瘤浸润淋巴细胞(TIL)治疗:转移性肺癌的潜在治疗策略
2021-08-16 xiaozeng MedSci原创
尽管PD-1免疫检查点抑制剂在转移性肺癌的治疗中已取得了一定的进展,但大多数患者未能达到客观的治疗反应。即使在联合一线铂类药物的双药化疗后,大多数患者在12个月内仍会出现疾病的进展。
尽管PD-1免疫检查点抑制剂在转移性肺癌的治疗中已取得了一定的进展,但大多数患者未能达到客观的治疗反应。即使在联合一线铂类药物的双药化疗后,大多数患者在12个月内仍会出现疾病的进展。
虽然目前的研究主要致力于鉴定新的免疫检查点组合,但迄今为止的相关临床结果均是渐进式的。非小细胞肺癌(NSCLC)作为免疫学上的一种“冷”肿瘤,缺乏激活的肿瘤特异性T细胞。因此,转移性NSCLC急需更有效的联合免疫治疗策略。
既往研究显示,肿瘤浸润淋巴细胞(TIL)的过继细胞疗法已在黑色素瘤的治疗中显示出活性,但目前尚未在转移性NSCLC中进行评估。
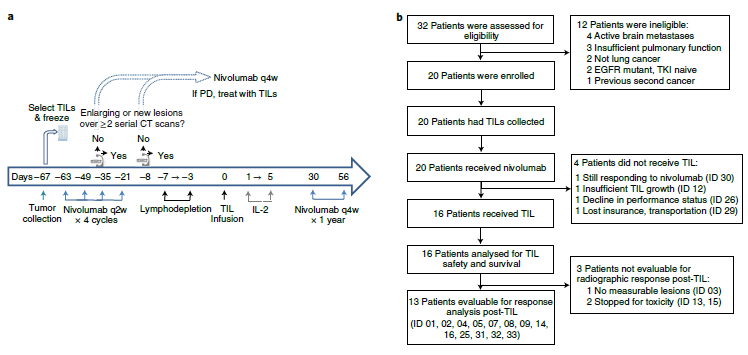
在该单臂开放性1期试验中,研究人员旨在评估20名在接受纳武单抗单药治疗后出现疾病进展的晚期非小细胞肺癌患者的TILs联合纳武单抗治疗的疗效。该试验的主要终点为治疗的安全性,次要终点包括客观缓解率、缓解的持续时间以及T细胞的持久性。
自体TIL是通过interleukin-2(白细胞介素2)培养切碎的肿瘤进行体外扩增的。患者接受环磷酰胺(cyclophosphamide)和氟达拉滨(fludarabine)进行淋巴细胞的清除、以及TIL和白细胞介素2的注射,随后接受纳武单抗的维持性治疗。
相关研究示意图
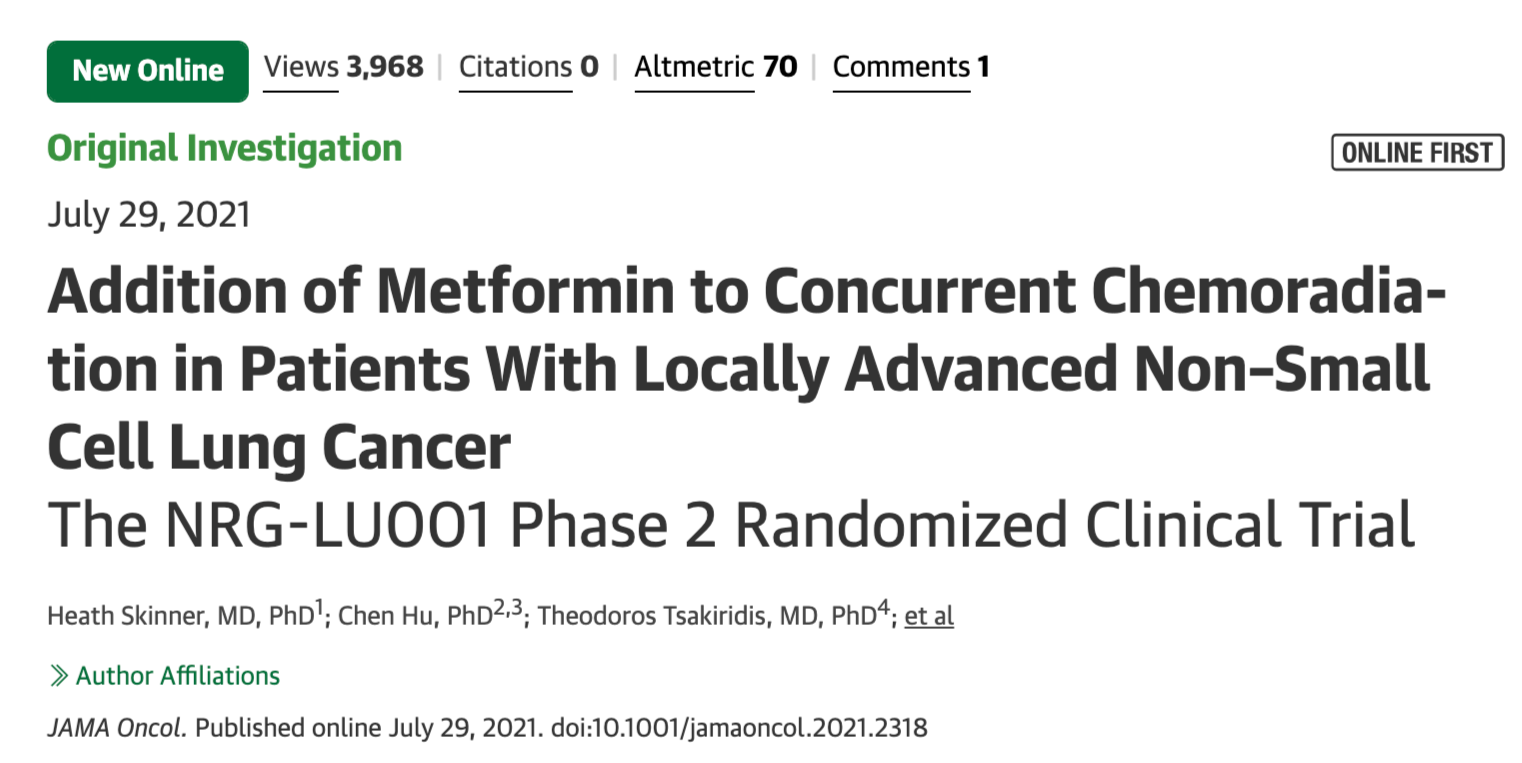
通过分析制定的≤17%的严重毒性发生率的预设标准,该试验最终达到安全性终点。在13名可评估的患者中,3名确认对治疗有反应,而11名患者出现肿瘤负荷的减少。研究人员发现,两名患者在1.5年的持续治疗后取得了完全缓解。
在探索性分析中,研究人员发现,在TIL治疗后可检测到识别多种类型癌症突变的T细胞,且在对治疗有反应的患者中富集。进一步的研究显示,新抗原反应性T细胞在治疗后患者的外周血中增加并持续存在。
TILs的临床活性与患者生存率分析
总而言之,该研究结果揭示,自体TIL细胞治疗通常是安全的且具有临床活性,其或可成为转移性肺癌潜在的新治疗策略。
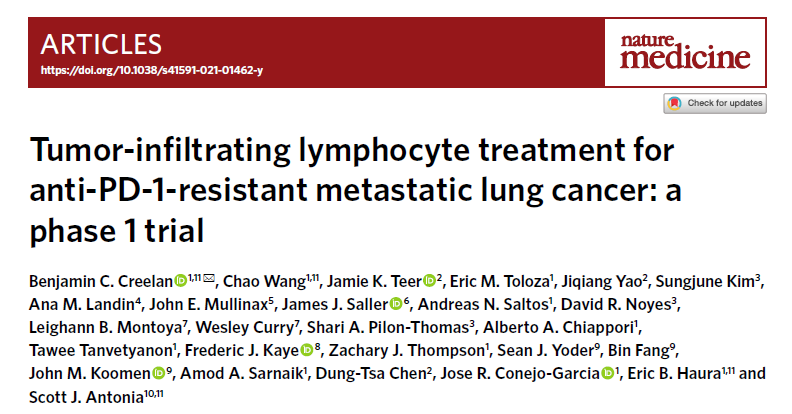
原始出处:
Creelan, B.C., Wang, C., Teer, J.K. et al. Tumor-infiltrating lymphocyte treatment for anti-PD-1-resistant metastatic lung cancer: a phase 1 trial. Nat Med 27, 1410–1418 (12 August 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
70
学习了#学习#
108
#淋巴细胞#
91
#转移性#
67
#Med#
0
学习
100
很精辟
100