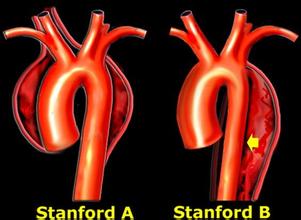
Circulation:复发性主动脉夹层(观察性研究)
2016-09-15 Mechront 译 MedSci原创
研究者通过国际急性主动脉夹层注册表数据库(IRAD),对目前复发性主动脉夹层(AD)患者的临床资料和预后进行了研究。 研究共纳入了204例复发AD患者,与3624例初发AD患者进行了比较,分析了患者特征、干预和结局。使用迭代Logistic模型,探索与复发AD有关的变量。使用Cox回归分析,探索与5年生存率有关的变量。对复发性AD患者的一个子集进行了解剖分析。 结果显示,复发性AD患者
研究者通过国际急性主动脉夹层注册表数据库(IRAD),对目前复发性主动脉夹层(AD)患者的临床资料和预后进行了研究。
研究共纳入了204例复发AD患者,与3624例初发AD患者进行了比较,分析了患者特征、干预和结局。使用迭代Logistic模型,探索与复发AD有关的变量。使用Cox回归分析,探索与5年生存率有关的变量。对复发性AD患者的一个子集进行了解剖分析。
结果显示,复发性AD患者更有可能患有马凡氏综合征(MFS)(21.5% vs. 3.1%, p<0.001),而不是二叶式主动脉瓣(BAV) (3.6% vs. 3.2%, p=0.77)。与初发AD患者相比,复发性AD患者的降主动脉尺寸更大,且与前哨解剖类型无关(A型 4.3 cm [3.5-5.6] vs. 3.3 cm [2.9-3.7], p<0.001; B型 5.0 cm [3.9-6.0] vs. 4.0 cm [3.5-4.8], p<0.001),尤其是MFS患者,这种联系更强烈。
在多变量分析中,诊断MFS是复发性AD的独立预测因素(HR 8.6,95% CI 5.8-12.8, p<0.001)。复发性AD患者中,近端AD后复发远端AD vs 远端AD后复发近端AD,患者年龄更小、更年轻(42.1 ± 16.1岁 vs 54.3 ± 14.8岁, p=0.004)。
结果表明,急性主动脉夹层患者中,5%的既往有主动脉夹层病史;复发性AD与MFS强烈相关。
原始出处:
Eric M. Isselbacher,et al.Recurrent Aortic Dissection: Observations from the International Registry of Aortic Dissection (IRAD).Circulation.published online before print September 1, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性#
54
讲的很好,谢谢分享
106
很好的内容,谢谢分享。
123
很好的内容,谢谢分享。
113
继续学习
94
继续关注
67
#主动脉#
43
#观察性研究#
57
#动脉夹层#
63
谢谢分享!
57