【病史临床】
女,61岁,咳嗽咳痰十余年,反复出现心悸、气促9年,加重两个月。
【影像图片】
胸部CT平扫纵隔窗(图A)、肺窗(图B);胸部正位平片(图C)

【影像表现】
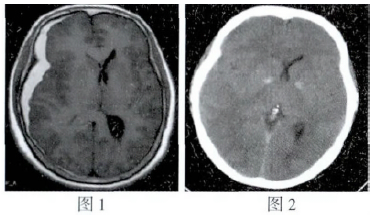
胸部CT平扫纵隔窗(图A)可见肺动脉主干及左右肺动脉主支明显增粗,肺窗(图B)示胸廓前后径增大,双肺透光度增加,肺纹理牵拉稀疏,并可见左下肺肺大泡形成。胸部正位X平片(图C)可见肺动脉段突出,右下肺动脉干明显增粗直径大于14 mm,周围肺野肺纹理稍稀疏,形成“残根征”。左心缘下段圆隆上翘。
【诊断】
慢性肺源性心脏病(根据患者多年慢支肺气肿的病史结合胸片和CT片可确诊)
【鉴别诊断】
1.高血压性心脏病;2.风湿性心脏病;3.肺源性心脏病
【讨论】
慢性肺源性心脏病(Cor Pulmonale)多数是发生在慢性支气管炎或肺气肿的基础上引起肺循环阻力增高,肺动脉高压, 导致右心肥大, 伴有或不伴有心力衰竭。病程一般在10年以上,早期多表现为咳嗽、咳痰、气喘等肺部疾病的症状与体征, 晚期则出现循环与呼吸衰竭的征象。肺气肿表现为桶状胸, 心尖搏动减弱。叩诊呈过清音, 肺下界下移等体征。右心衰竭时有颈静脉怒张, 心率增快, 剑突下可听到奔马律及来自房室瓣(三尖瓣) 关闭不全的收缩期杂音, 肺动脉第二音亢进。肝大、腹水、下肢水肿等。
影像诊断要点
X线表现:慢性支气管炎可见双肺纹理增多、增粗、边缘模糊,以双下肺明显。肺气肿表现为肋骨走行水平, 肋间隙增宽,双肺透光度增加, 肺纹理纤细稀疏,双侧膈肌下降, 活动幅度小。肺动脉高压表现为肺动脉段凸出,左右肺动脉及其分支扩张, 以右下肺动脉第1分支最为明显,表现为后前位胸片自肺门角向下约1 cm处, 右下肺动脉直径大于15 mm为扩张的阳性指征。周围肺野动脉骤然变细,形成“残根征”。右心室肥厚,表现为左心缘下段圆隆上翘,但因常合并肺气肿,故心胸比例不大。晚期可见右心缘向右凸。
CT或MRI: 胸部CT肺窗示肺纹理稀疏、紊乱,肺部密度降低,并可合并肺大泡,胸廓前后径增大。纵隔窗示肺动脉主干和左右肺动脉主支明显增粗,肺动脉主干直径大于30mm。增强扫描可见右心室壁增厚,大于左心室壁厚度的1/2。MRI SE序列T1WI可见主肺动脉内出现血流高信号提示有肺动脉高压,增强可见右心室壁厚度大于5mm,可等于或超过左心室壁厚度,室间隔向左心室侧凸出,右心房亦可扩大,腔静脉扩张,晚期,左心房室亦扩张CRE序列MRI可见三尖瓣(收缩期)和肺动脉瓣(舒张期)的返流,同时可直观地反映右心室收缩和舒张的功能。
对于该病,X线平片、CT、MRI等影像表现是非特异的,必须结合病史及心肺功能的试验室检查方可确诊。
【问题】
Ture OR False?
1.X线平片(图C)可示主动脉结增大; 对: 错
2.X平片示肺动脉段突出; 对: 错
3.CT扫描肺窗(图C)示肺纹理增多,肺透光度降低; 对: 错
4.CT平扫纵隔窗(图A)示肺动脉主干及左右主支增粗。 对: 错
正确答案: 1:× 2:√ 3:× 4:√
关于该病例的影像叙述错误的是?
A.CT胸部扫描可见胸廓前后径变窄,肺透亮度降低,肺部以炎性渗出为主;
B.X平片上可见肺动脉段突出,肺动脉主干、左右主支明显扩大,周围肺野动脉骤然变细,形成残根征;
C.CT胸部扫描可见胸廓前后径增宽,肺窗示肺透亮度增高,左肺还可见肺大泡形成;
D.CT平扫纵隔窗示肺动脉主干及左右主要分支明显增粗。
正确答案:A
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肺源性心脏病#
63
#CT病例#
63
学习学习.知之为知之
112
#X线#
69
#影像诊断#
76
一起学习学习
92
学习了.获益匪浅.
97