BMJ:老年人因“象牙脊椎”引起的胸背部疼痛-案例报道
2016-11-24 haofan MedSci原创
在整个椎体中硬化症表现的特别明显,但椎体没有出现膨胀或骨折,而且这是一个孤立的病变。引起这种影像学变化的原因包括前列腺癌、乳腺癌和淋巴瘤的转移病灶。
患者为76岁的男性,伴有前列腺癌病史,因中胸背部疼痛逐渐加剧而就诊,胸椎X线片结果如下(图1),影像学结果显示为何?

图1 胸椎X线片
答案:X线平片显示硬化的T6椎体(图2,箭头),这种影像学表现有时被称为“象牙脊椎”。
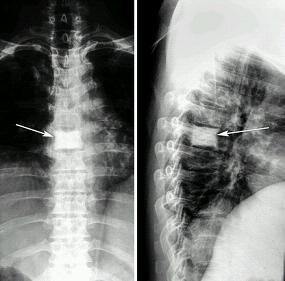
图2 胸部平片显示硬化的T6椎体(箭头),这种影像学表现有时被称为象牙脊椎。
讨论
在整个椎体中硬化症表现的特别明显,但椎体没有出现膨胀或骨折,而且这是一个孤立的病变。引起这种影像学变化的原因包括前列腺癌、乳腺癌和淋巴瘤的转移病灶。佩吉特病也应该予以考虑,尽管它通常会导致椎体扩大。由于这名男子有前列腺癌的病史,前列腺癌转移是最有可能的原因。磁共振检查能提供病变特点更详细的信息,并有助于寻找隐匿性脊柱病变。骨扫描检查也应进行,以寻找其他地方的病变。检查结果发现这个病人的肋骨和骨盆也有病变累及。
结局
患者开始雄激素剥夺治疗,但预后较差。
原始出处:
Joseph Dalby Sinnott,et al. An older man with thoracic back pain. BMJ.23 November 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
40
#胸背部#
65
涨姿势了
71
#脊椎#
67