Prostate Cancer P D:水蒸气热疗能够减轻导管依赖的尿滞留
2019-12-03 AlexYang MedSci原创
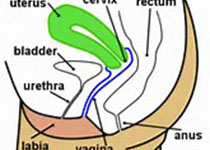
水蒸汽热疗通过利用对流传递的热能来靶向消融阻塞性前列腺组织。最近,有研究人员报道了该热疗方法在减轻与良性前列腺增生(BPH)相关的非神经性尿滞留上的结果情况。研究人员对38名导管依赖的男性进行了回顾性的分析,他们的平均年龄为75.5岁。研究发现,在治疗的38名患者中,1名患者在跟踪调查时丢失,剩下的37名中的26名(70.3%)能够自发的排尿(TWOCs均值为1.6±0.8),且热疗后不依赖导管的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
60
#热疗#
116
#ROS#
67
#PRO#
47