解放军总医院发布CAR-T疗法 I期临床数据
2015-05-27 佚名 生物探索
近日,Cellular Biomedicine Group宣布了其CAR-T CD30霍奇金淋巴瘤免疫-肿瘤研发项目令人振奋的I期临床数据。7名患者中有5人对CAR-CD30 T细胞疗法有应答,且该疗法被证明安全、可行、有效。 该试验由中国解放军总医院设计并执行,项目主要负责人是该院癌症免疫治疗部门的主任韩卫东教授。该研究招募的患者具有严重的治疗历史和/或多个肿瘤病变却没有可用的

近日,Cellular Biomedicine Group宣布了其CAR-T CD30霍奇金淋巴瘤免疫-肿瘤研发项目令人振奋的I期临床数据。7名患者中有5人对CAR-CD30 T细胞疗法有应答,且该疗法被证明安全、可行、有效。
该试验由中国解放军总医院设计并执行,项目主要负责人是该院癌症免疫治疗部门的主任韩卫东教授。该研究招募的患者具有严重的治疗历史和/或多个肿瘤病变却没有可用的治疗方案,即现在的疗法下只有有限的预后(several months to < 2 year survival)。
7名患有复发/难治性霍奇金淋巴瘤的患者参加了CAR-CD30 T细胞疗法试验,其中2人获得部分缓解,3人获得疾病稳定(stable disease ,SD),因此,该疗法整体疾病控制率为71.4%(5/7);客观缓解率为28.6% (2/7)。此外,此疗法对其中1人产生了副作用,细胞回输2周后产生了5天的self-limiting关节痛、肌痛和双膝肿胀。
5月21日,在英国伦敦举行的第十届世界干细胞与再生医学大会,Cellular Biomedicine Group的首席执行官William (Wei) Cao公布了这些数据。他说:“CAR-T CD30技术的有效性和安全性数据让我们备受鼓舞。”
不久前, Wei (William)Cao还在Regen医学投资者大会上公布了该公司另外两种CAR-T细胞疗法的I期临床结果。CAR-CD19 T实验招募了9个复发或化疗难治性B细胞急性淋巴细胞白血病(ALL)的成人患者。结果发现22.2%的患者(2/9)表现完全缓解和44.4%的患者(4/9)显示部分缓解,总缓解率为66.7%(6/9)。
CAR-CD20 T实验有7例化疗难治性,晚期弥漫性大B细胞淋巴瘤(DLBCL)患者参与,其中2个含有大块肿瘤患者当中的1个经CAR-CD20T细胞治疗后在14个月内显示完全缓解,另一例6个月内表现部分缓解。4个有效大块肿瘤负荷病例当中的3个治疗后取得3至6个月缓解,总应答率75%(3/4)。
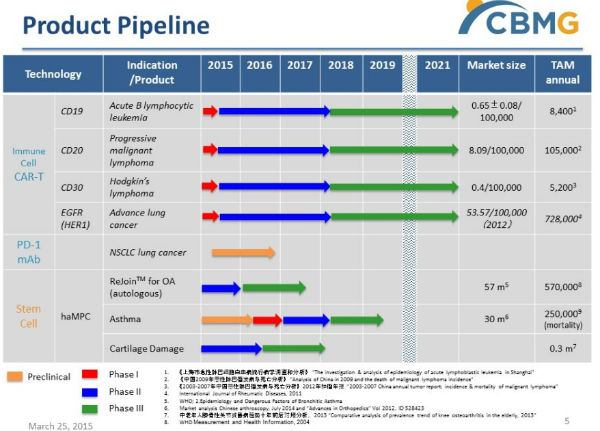
Cellular Biomedicine Group产品线
Cellular Biomedicine Group是一家在纳斯达克上市的致力于研发治疗退行性疾病和癌症细胞疗法的公司。2月9日,该公司收购了中国解放军总医院的CAR-T细胞疗法,这项收购包括CD19、CD20、CD30、以及人表皮生长因子受体(EGFR)重组表达载体等免疫技术,已有的临床I/II期结果、相关专利的所有权、以及生产技术。
Wei (William)Cao表示,公司希望能够在今年的第三季度公布EGFR-HER1-阳性晚期肺癌试验的临床数据,并获得Immuno-Oncology平台中其它项目的进一步进展。
原始出处:
Cellular Biomedicine Group Announces Positive Phase I Results From CAR-T CD30 Immuno-Oncology Clinical Development Program
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床数据#
67
#I期临床#
77
#CAR-#
89
#解放军总医院#
72
#总医院#
73
看看
202