《中国血糖监测临床应用指南2015版》解读
2016-02-03 陈莉明 国际糖尿病杂志
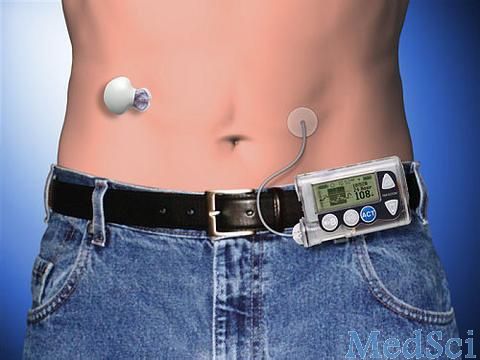
作者:天津医科大学代谢病医院院长 陈莉明教授 血糖监测是糖尿病管理中的重要组成部分,《中国血糖监测临床应用指南(2015年版)》新增了血糖监测的治疗原则、院内床边快速(Point of care testing,简称POCT)血糖监测和实时动态血糖监测,突出了POCT和根据患者实际情况制定血糖监测方案的重要性。明确了ISO15197-2013标准评价血糖仪的精准性。同时,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床应用#
67
值得学习
166
值得学习
114
值得学习
135
值得学习
140
值得学习
124
值得学习
76
值得学习
90
值得学习
165
值得学习
115