DES未能降低较大直径冠脉病变患者的TVR风险
2012-04-17 高晓方(译) 医学论坛网
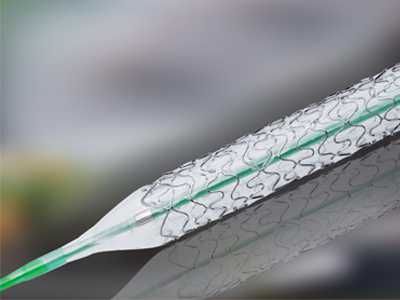
最近,美国学者的一项研究表明,在伴有较大直径冠脉病变的患者中,与金属裸支架(BMS)相比,药物洗脱支架(DES)未能降低靶血管血运重建(TVR)风险。论文发表于《美国心脏病学会杂志》[J Am Coll Cardiol 2012, 59:198]。 随机试验显示DES在降低TVR风险方面优于BMS,但此种获益随动脉直径增加而减弱。目
最近,美国学者的一项研究表明,在伴有较大直径冠脉病变的患者中,与金属裸支架(BMS)相比,药物洗脱支架(DES)未能降低靶血管血运重建(TVR)风险。论文发表于《美国心脏病学会杂志》[J Am Coll Cardiol 2012, 59:198]。
随机试验显示DES在降低TVR风险方面优于BMS,但此种获益随动脉直径增加而减弱。目前尚不清楚在临床实践中DES对于较大冠脉是否优于BMS。此项研究的资料来自于NHLBI动态登记的869例患者;受试者均接受参考血管直径≥3.5 mm的新发病变经皮冠脉介入术(PCI)。依据受试者是否接受DES或BMS治疗对数据加以分析。就心血管事件发生情况对患者进行为期3年的随访。
结果显示,与BMS患者(299例)相比,DES患者的高血压、高脂血症和肾病患病率较高,既往接受冠脉介入治疗的比率亦较高。随访第3年时,DES和BMS组患者的未校正死亡率相似,分别为8.6%和9%。第3年时DES组患者存在过量心梗(MI)趋势(7.8%对3.9%,P=0.05)。两组患者在第3年时TVR率均较低并且基本相似(4.4%对3.7%)。对基线特征进行校正之后,DES的第3年MI校正风险比为1.85,第3年TVR和死亡校正风险比分别为1.14和0.89。
链接:COMPARISON OF BARE-METAL AND DRUG-ELUTING STENTS IN LARGE CORONARY ARTERIES: A REPORT FROM THE NATIONAL HEART, LUNG, AND BLOOD INSTITUTE DYNAMIC REGISTRY
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#冠脉病#
72
#冠脉病变#
69
#DES#
82
#DES#
77