细胞治疗传来喜讯:Kite Pharma发布KTE-C19临床II期试验部分结果,治疗侵袭性淋巴瘤的缓解率为76%,疗效明显
2017-03-01 板栗 医麦客
Kite Pharma公司在2017年 BMT Tandem会议期间提交了ZUMA-1 II期试验的部分中期分析,在随访一个月后发现,接受CAR-T细胞治疗的非霍奇金淋巴瘤(NHL)的患者中有76%的客观缓解率(ORR)和47%的完全缓解率(CR)。FrederickL. Locke,MD主要研究者FrederickL. Locke,MD公布,3个月的持续完全应答率(CR)为39%,比历史对照

Kite Pharma公司在2017年 BMT Tandem会议期间提交了ZUMA-1 II期试验的部分中期分析,在随访一个月后发现,接受CAR-T细胞治疗的非霍奇金淋巴瘤(NHL)的患者中有76%的客观缓解率(ORR)和47%的完全缓解率(CR)。

FrederickL. Locke,MD
主要研究者FrederickL. Locke,MD公布,3个月的持续完全应答率(CR)为39%,比历史对照要高出6倍。在99%的病例中成功制备了Axicabtagene ciloleucel,从血浆分离到临床的过程中,平均经过17天。该研究涉及了22个病例。
Locke说:“这是 CAR-T细胞治疗在难治性侵袭性NHL中的第一个关键的多中心研究。ZUMA-1的关键结果与早期研究结果一致。这包括单中心NCI研究,12个月完全缓解率为44%和47%。 ZUMA-1的I期部分在12个月的完全缓解率为43%,持久性不错。”
研究表明,不良事件管理可以在22个病例中有效实施,H. Lee Moffitt癌症中心,血液和骨髓移植和细胞免疫治疗,研究员Locke说,大多数患者没有CAR-T细胞治疗经历。
大量患者水平的meta分析(SCHOLAR-1研究)显示,对最后一线化疗没有反应的最多具有稳定的疾病或进行性疾病,或者在自体造血干细胞移植后12个月内复发的患者,对二线治疗具有26%的ORR和8%的CR。患者的总生存期为6.6个月。
Locke说:“这些患者确实没有良好的治疗选择,需要新的治疗方式”。ZUMA-1的I期结果在12个月的完全缓解率持续为43%。
II期研究包括2个小组,小组1的弥漫性大B细胞淋巴瘤(DLBCL)患者和小组的原发性纵隔B细胞淋巴瘤(PMBCL)和滤泡性T细胞淋巴瘤的患者。患者具有化疗性免疫疾病,并且最多达到稳定的疾病或进行性疾病作为对其最后一线化疗的反应,或者它们在先前的自体移植的12个月内复发。II期部分的主要终点是ORR。当对小组1中的50名患者进行至少3个月的随访时,触发中间分析。
总的来说,111名患者入组接受白细胞分离术,其中110名患者有足够的细胞制备CAR-T细胞。患者接受氟达拉滨和环磷酰胺预处理,101名接受axicabtagene ciloleucel(CAR-T药物KTE-C19)。对93例患者进行了至少1个月的随访,其中62例患者进行了至少3个月的随访。
参与者的中值年龄为59岁,约一半的患者为60岁或以上。以前治疗的中位数为3,多达12个接受。在44%的患者中,国际预后指数(IPI)为3至4。约80%的患者通过化疗难以治愈,其余的患者在先前的自体移植的12个月内出现了复发的情况。
Axicabtagene ciloleucel(KTE-C19)诱导快速反应,在第一次肿瘤评估(输注CAR-T细胞后30天)最明显。在1个月随访的93例患者中,71%有反应,38%有CR。后续的实验正在进行中。
在3个月的时间点,总体反应率为39%。有7名患者在3个月时转为CR,1个月时有稳定的疾病或部分反应。移植后复发的患者的完全缓解率为75%(12名患者中的9名)。
中期分析的93名患者中,92%出现了3级或以上不良事件。这些中的大多数是与氟达拉滨和细胞毒性化学疗法相关的血液毒性。19%的患者中,脑病是神经学事件的最常见的表现,最常见的3级或以上不良事件是中性粒细胞减少症(63%),贫血(42%),白细胞减少症(40%)和发热性中性粒细胞减少症(29%)。
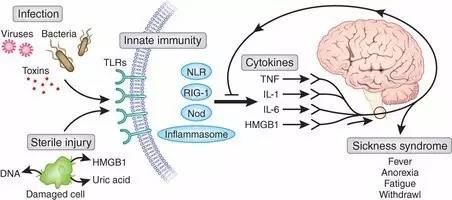
13%的患者遭遇了3级(严重)或以上(威胁生命)细胞因子释放综合征(CRS),29%的患者出现了3级或以上神经病学事件。为了治疗这些事件,38%的患者接受tocilizumab,17%的患者接受皮质类固醇,17%的患者接受两者。将进行性疾病排除在外有3个致死事件,嗜血细胞性淋巴组织细胞增多症;在CRS环境中的心脏停搏;肺栓塞。没有脑水肿病例。
Locke说CRS和神经系统事件通常是可逆的。除了在CRS环境中的心脏停搏外,所有的CRS事件已经解决了。在数据截止时有三个神经学事件正在进行。
另外的分析显示在外周血中评价CAR-T细胞水平;在3个月时CR的患者的CAR-T细胞水平中值比在3个月时不在CR的患者高出6倍。类似地,3级或更高级神经系统事件的患者的CAR-T细胞水平中值是2.5倍。CAR-T细胞扩增峰值发生在7到14天之间。
在血清中测量了四十六种细胞因子和趋化因子。在3级或更高级的CRS和3级或更高级的神经系统事件的患者中观察到IL-15和IL-6水平升高。在3级或更高CRS的患者中IL-2受体α和IL-10水平升高,但在3级或更高级神经系统事件的患者中却截然不同。
KTE-C19针对的适应症为不适合自体干细胞移植的复发/难治侵袭性B细胞非霍奇金淋巴瘤(NHL)的患者。
Kite Pharma:axicabtagene ciloleucel
KTE-C19是一种在研的嵌合抗原受体T-细胞治疗技术,经基因工程改造的患者自体T细胞可靶向作用于B细胞淋巴瘤和白血病表面的CD19抗原。2015年12月KTE-C19用于DLBCL、PMBCL、FL获得FDA的突破性药物资格认定。KITE还计划于2017年向EMA提交该药物新药申请,2016年6月,KTE-C19 用于难治性DLBCL获得了EMA的”优先药物“资格。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Pharm#
62
#pharma#
61
#II期试验#
55
看上去还行!
72
#侵袭性#
55
#KIT#
71
相当牛的疗效!
74