男性,45岁,因出现发热和黄疸4天余加重来院急诊就诊。
经初步检查后发现,该男子白细胞增多,转氨酶升高,表明可能患上了胆管炎。
会诊医师对其使用广谱抗生素治疗,但患者症状没有明显改善的迹象。
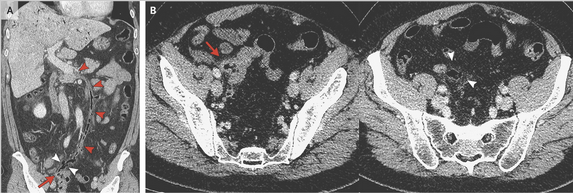
CT扫描显示乙状结肠憩室炎急性穿孔(如图A和B箭头处)和肠系膜存在气体(图A和B白色箭头处)。另外,在肠系膜下静脉延伸至脾静脉到门静脉的起源出发现有气体(图A红色箭头所示),这一发现是符合门静脉炎的临床诊断。
为了能尽快控制该男子的病情,会诊医师决定对其进行紧急Hartmann’s 手术,并应用抗生素进行抗感染治疗。
术后,该男子的临床症状有明显的的改善,并在术后的第18天办理出院。
门静脉炎通常与腹腔内各器官及组织静脉化脓性血栓形成有关,如憩室炎,阑尾炎,胰腺炎,炎症性肠病等。
其中,脆弱类杆菌和大肠杆菌是其最常见的病原菌。
原始出处:
Fernando Bazan, M.D., and Marcos Busto, M.D.Pylephlebitis as a Complication of Diverticulitis,N Engl J Med 2015
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#并发#
70
谢谢分享。
147
谢谢分享。
144
这篇文章有一定深度
100
是一篇不错的文章
182
值得临床关注
140
不错,赞一个
127
赞
86
好文章,值得收藏
122
这个也能发表文章??
116