ISC 2018:DEFUSE 3研究全新结果:拓宽血管内血栓切除术应用时间窗新证据
2018-02-04 国际循环编辑部 国际循环
2018年国际卒中大会上发布的DEFUSE 3研究最新结果显示,CT/MR发现的具有可挽救组织的、大脑中动脉(MCA)和/或颈内动脉(ICA)闭塞的卒中患者在发病6~16小时内可从血管内血栓切除术中获益,这无疑为拓宽血管内血栓切除术在卒中患者中应用的时间窗提供了最新证据支持。
美国当地时间1月24~26日,2018年国际卒中大会(International Stroke Conference)在美国加利福尼亚州洛杉矶会议中心隆重举办。会上发布的DEFUSE 3研究最新结果显示,CT/MR发现的具有可挽救组织的、大脑中动脉(MCA)和/或颈内动脉(ICA)闭塞的卒中患者在发病6~16小时内可从血管内血栓切除术中获益,这无疑为拓宽血管内血栓切除术在卒中患者中应用的时间窗提供了最新证据支持。
研究简介
DEFUSE 3研究共计入选296例美国国立卫生研究院卒中量表(NIHSS)评分≥6分、卒中前改良Rankin量表评分为0~2、伴有ICA和/或MCA闭塞且RAPID软件定量评估显示最大梗死核心≤70 ml的卒中患者,将其随机分配至血管内血栓切除术组和单纯药物治疗组。研究的主要终点是位移分析所示的干预90天后的改良Rankin量表评分变化情况。鉴于同类研究DAWN研究于2017年5月获得阳性结果,故研究者对该研究进行了中期分析。
中期分析主要结果
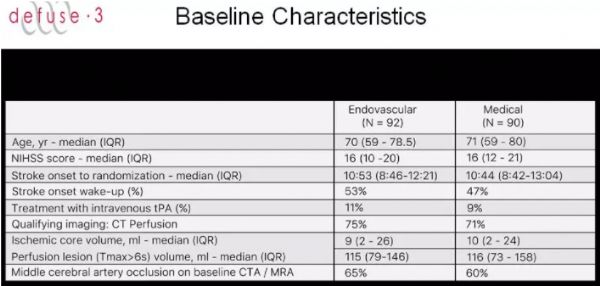
对来自38家中心的182例患者(血管内血栓切除组92例,药物治疗组90例)一年结果的中期分析发现,两组患者的基线特征无显著差异(图1)。
图1. 两组患者的基线特征
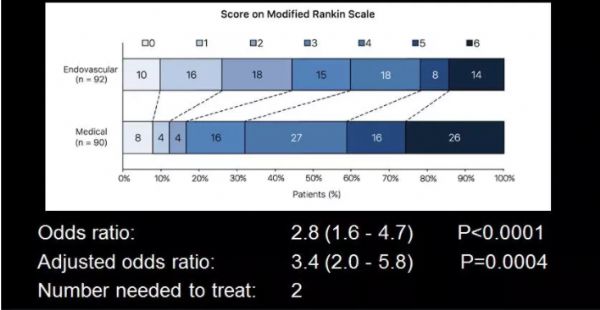
进一步分析发现,与药物治疗组相比,血管内血栓切除术组患者的改良Rankin量表评分显著改善(OR及校正后OR值分别为2.8和3.4,NNT=2,见图2);改良Rankin量表评分为0~2分者的比例更高(45% vs.17%,P<0.0001),改良Rankin量表评分为5~6分者的比例更低(22% vs.42%,P=0.0048)。此外,与药物治疗组相比,血管内血栓切除术组患者实现再灌注及再通者的比例均更高(79%vs. 18%和78%vs. 18%,P均<0.0001)。就安全性而言,与药物治疗组相比,血管内切除术组患者症状性颅内出血发生率并无显著差异(6.5%vs.4.4%,P=0.75),死亡率有降低趋势(14%vs.26%,P=0.05)。
图2. 两组患者的主要终点
中期分析亚组分析结果
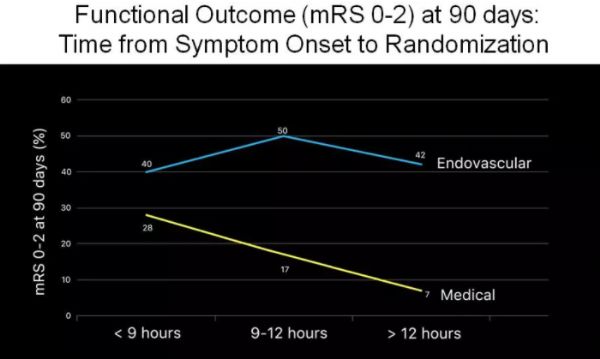
该研究中62%的患者符合DAWN研究的入选标准,亚组分析显示,符合DAWN研究标准的患者中,与药物治疗相比,血管内血栓切除术改善改良Rankin量表评分的OR值为2.7(95%CI:1.4~5.2);不符合DAWN研究标准的患者中上述OR值为3.0(95%CI:1.3~7.0)。对起床时发作者及目击者发现的患者进行亚组分析发现,前者中前述OR值为3.4(95%CI:1.6~7.4),后者中前述OR值为3.4(95%CI:1.4~8.3)。根据随机化时间行亚组分析发现,症状发作至随机化的时间超过11小时者中前述OR值为5.7(95%CI:2.4~13.1),≤11小时者中前述OR值为1.7(95%CI:0.9~3.4)。90天时的功能性结局(Rankin量表评分为0~2),分析显示,症状发作至随机化的时间不同与药物治疗相比血管内血栓切除术改善功能结局的优势有所差异(图3)。
图3. 症状发作至随机化的时间对两组患者功能结局的影响
综上可见,DEFUSE 3研究延长了卒中患者行血管内血栓切除术患者的时间窗,有助于让更多患者从上述治疗中获益。该研究对于相关指南制定产生了直接影响,对于卒中患者的影像学检查、分类救治及治疗也将产生实质性影响,并为我们认识“时间就是大脑”提供了新视角。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
59
#DEFUSE#
72
#血栓切除#
53
#血栓切除术#
84
#血管内血栓切除术#
60
#ISC#
59
学习
83