松果体区非典型性囊性脑膜瘤一例
2019-02-27 许珂 张勇 程敬亮 临床放射学杂志
患者女,54岁。以“头痛、头晕半年,记忆力减退20余天”为主诉入当地医院,为求进一步诊治,到本院就诊,体检:意识清楚,精神一般,记忆力减退,计算力减退,四肢肌力5级,双侧跟膝胫试验欠稳准,Romberg征阴性,双侧病理征阴性。
患者女,54岁。以“头痛、头晕半年,记忆力减退20余天”为主诉入当地医院,为求进一步诊治,到本院就诊,体检:意识清楚,精神一般,记忆力减退,计算力减退,四肢肌力5级,双侧跟膝胫试验欠稳准,Romberg征阴性,双侧病理征阴性。
头部MRI平扫显示:松果体区可见巨大团块状稍长T1、稍长T2信号,病变信号欠均匀,其内可见片状更长T1(图1)、更长T2信号(图2),DWI高b值轻度扩散受限(图3),小脑及中脑受压变形。增强显示:松果体区及四叠体池病灶可见不均匀明显强化,大小约4.5 cm×4.0 cm×4.5 cm(前后径×左右径×上下径)(图4、5)。诊断:松果体区巨大占位性病变,考虑松果体脑膜瘤。
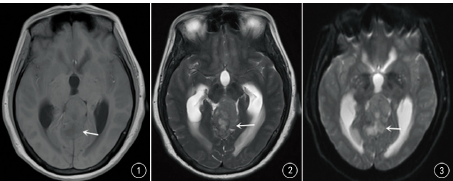

图1头部MRI轴位T1WI可见松果体区巨大团块状稍长T1信号,病变信号欠均匀,其内可见片状更长T1信号;图2头部MRI轴位T2WI松果体区可见巨大团块状稍长T2信号,病变信号欠均匀,其内可见片状更长T2信号;图3头部轴位DWI呈高b值轻度扩散受限;图4头部MRI轴位增强显示松果体区病灶可见不均匀明显强化;图5头部MRI矢状位增强显示松果体区病灶可见不均匀明显强化
术中可见:肿瘤体积大,呈红白色,质韧,边界清楚,血运丰富。术后病理学肉眼所见:灰黄灰红碎组织一堆,切面灰白质中。镜下可见:瘤细胞较密集,呈片状分布,细胞周界不清呈合体状,常无明确构形,胞核密集较大,呈圆形、卵圆形,核质比例增大。免疫组织化学结果:CK(-),EMA(灶+),Vimentin(+),GFAP(-),S-100(-),PR(灶+),CD34(-),Bcl-2(部分+),CD99(部分+),Oligo-2(-),Ki-67(约20%+)。病理诊断:(松果体区)非典型性脑膜瘤,WHOⅡ级(图6)。

图6 囊性非典型性脑膜瘤病理图(HE×200):细胞密集呈片状分布,细胞周界不清呈合体状,胞核密集,核质比例增大
讨论
脑膜瘤是常见的起源于脑外的良性肿瘤,50%位于矢状窦旁,另大脑凸面、大脑镰旁者多见,典型的表现为实质性肿块,具有特征性的CT和MRI影像学表现。脑膜瘤原发于蛛网膜内皮细胞,凡属颅内富于蛛网膜颗粒与蛛网膜绒毛之处皆是脑膜瘤的好发部位,松果体区脑膜瘤比较少见,占所有松果体区肿瘤的6%~11%。具有肉眼可见的囊变和(或)坏死的脑膜瘤为囊性脑膜瘤,脑膜瘤多属于良性肿瘤,通常呈实质性,组织分化良好,生长缓慢,囊性脑膜瘤发病率极低,约占脑膜瘤的1.6%~10.0%。
Nauta分型将囊性脑膜瘤分为4型:Ⅰ型:囊腔位于肿瘤的深部或中央,周围完全被肿瘤所包绕;Ⅱ型:囊腔位于瘤内靠近肿瘤边缘(远颅内侧);Ⅲ型:囊腔包围肿瘤且位于周围脑组织内;Ⅳ型:囊腔包围肿瘤位于肿瘤与脑组织之间。本例应为Ⅰ型,即囊腔位于肿瘤内部。
囊性脑膜瘤MRI表现实性部分多信号均匀,增强扫描实性部分明显强化,有时可见“脑膜尾征”。肿瘤内囊性变的原因可能为肿瘤细胞变性导致微囊形成,后微囊融合形成肿瘤内囊腔;或是坏死灶转变为囊腔。松果体区囊性非典型性脑膜瘤较少见,诊断具有一定困难,有时较难与松果体内其他肿瘤相鉴别,如生殖细胞瘤、成人髓母细胞瘤。生殖细胞瘤MRI表现T1WI为稍长信号或等信号,T2WI常呈等信号或稍长信号,增强后呈明显均匀一致强化,并能发现沿脑脊液或室管膜转移的病灶。成人髓母细胞瘤易囊变,且病变常累及脑膜引起脑膜强化,表现很像囊性脑膜瘤,但增强后多数呈轻中度强化。诊断时应予以注意。
原始出处:
许珂,张勇,程敬亮,汪卫建.松果体区非典型性囊性脑膜瘤一例[J].临床放射学杂志,2018,37(01):36-37.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#非典型性#
62
#松果体#
88
#松果体区#
61
#囊性#
68
#脑膜瘤#
59
#非典型#
61