患者男性,27岁, 5月2日急诊就诊。
主诉:发热10天,咳嗽、咳痰伴左侧胸痛5天。患者10天前受凉后出现发热,其最高温度达39.5℃,呈持续高热,无寒战,无恶心呕吐、无尿频、尿急、尿痛等伴随症状。高热后曾自行口服“百服宁”1片,汗出后体温能下降到38℃以下,接近37℃,但仍然处于低热之中。第3天到当地村卫生所就诊,给予静滴“抗生素(具体名称不详)”2天,低温时退时升。继之出现咳嗽、咳痰,痰为白色稍黏稠,同时出现左侧胸痛,深呼吸时左侧胸痛明显。第5天行正位胸部X线,提示“左侧肺炎”,予“左氧氟沙星+阿奇霉素”抗炎以及“沐舒坦”化痰等治疗共治疗3天,患者症状没有减轻,仍反复发热,体温波动在38.5~395℃之间,经“赖安比林”肌注之后缓解,3-4小时之后再次发热,而且咳嗽不断,胸痛加剧,正常呼吸时即明显左侧胸痛。为此,调整抗生素为“倍能(国产美罗倍南)1g,每8小时1次,西普乐0.2g,每2小时1次”,其他辅助治疗。
既往体健,无传染病及接触史、家中务农,发热期间,家属中无类似发热病史。
通过询问,可知患者在受凉情况下出现高热,经过自行服药退热,病情没有得到控制反而进一步发展。在健康体格前提下受凉发热,继之嫩、痰和胸痛,考虑“呼道感染性发热”,但是经过相应的抗炎治疗,效果不明显甚至加重。是否存在抗炎治疗不对症,或者存在其他非感染性发热因素等,值得进一步思考。
体格检查:
由于患者发热并发咳嗽、咳痰和胸痛,考虑呼吸道感染性发热,因此重点检查为呼吸系统。当然,对于反复发作的发热,在考虑感染性发热的同时,对于年轻人,不要忽略非感染性发热的可能性。
体检结果:
当时查体:T38.5℃,P15次/分,R24次/分,BP105/65mHg。神清语利,偏瘦体形;倦怠,急性热病容。全身无明显皮疹;双侧巩膜无黄染,眼球活动正常;无颈静脉怒张,呼吸急骤,频率24次/分,深呼吸左侧胸痛明显,双侧胸部叩诊无明显浊音,双肺呼吸音粗,双下肺可闻及湿性啰音;心率115次/分,律齐,各瓣膜听诊区未闻及杂音;腹平软,全腹无压痛,肝脾肋下未及, Murphy征(-),移动性浊音(-),肠鸣音正常存在;双下肢无水肿;四肢肌力正常、双侧对称,双巴氏征阴性。
思维提示:
患者体格检查明癞提示呼吸系统存在问题,主要表现为下呼道感染征象。而非感染性发热的可能性不大。
实验室和影像学检查结果
(一)初步检查内容及目的
1.血常规常规检查根据白细胞等变化,初步判断感染的存在(注意与外院血常规对比)。
2.心电图急诊室常规检查,可了解是否合并心脏方面改变。
3.血气分析及电解质了解通气与换气的情况。
4.D-二聚体急诊除外血栓栓塞性疾病可能。
5.肺部HRCT患者转院之前已经携带当地胸部X线片,因此,直接选择胸部CT检查以便详细了解肺部情况。
(二)检查结果及思维提示
1.心电图窦性心动过速,无ST-T等方面改变。
2.血常规WBC4.39×109/L,N80.1%,HGB134g/L,PLT254x109/L。
3.血气及电解质pH7.531,PaCO223.3mmHg,PaO254.5mmHg(文丘里吸氧10L/min,FiO250%),PaO2/ FiO2=109;Na+134.4mmo/L, K+3.4 mmo/L ,Ca2+2.25mmo/ L, PHOS 0.93mm /L ,Glu7.75 mmol/l,其他均正常。
4.D-二聚体125ng/ml。
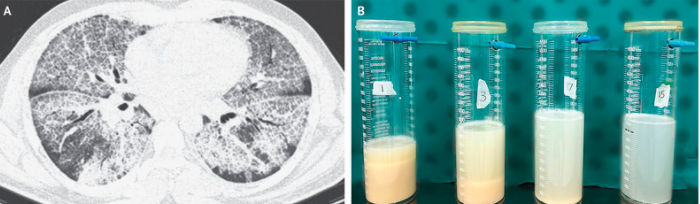
5.HRCT左侧大片实性改变,右侧渗出性改变。
思维提示:
血常规检查WBC正常,中性粒细胞升高。动脉血气分析为严重低氧血症,生化检查轻度低钠。主要改变为肺部,CT提示左肺大片状实性改变。考虑社区获得性肺炎。
(三)进一步检查结果
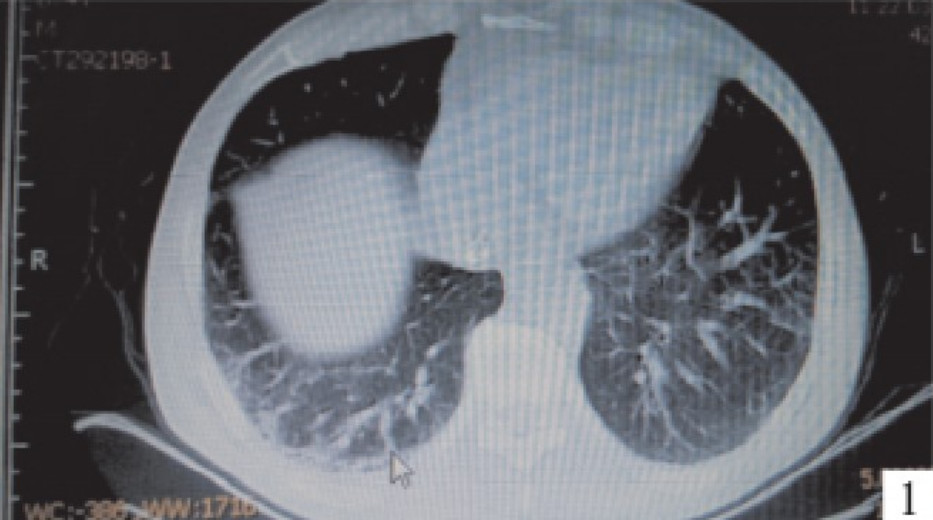
考虑患者为社区获得性肺炎,已经治疗5天,根据病史提供,抗菌治疗较为规范,抗菌谱覆盖的面也比较广,但是,却没有达到治疗的效果,而病情还在继续发展。因此,寻找病原学证据成为当务之急。而快速简便并且能完成的检查包括PCT(降钙素原)病毒核酸检测以及痰涂片检査。以上检查均只需要几十分钟到2小时不等的时间即可得到检査结果。而尿、痰和血培养病原微生物的结果至少需要3天以上时间才会有初步结果。因此,该患者在就诊当天就完成了PCT检测、气道分泌物痰涂片检查和病毒核酸检查。
结果如下:
PCT:0.26ng/ml;痰病毒核酸检验:腺病毒(+),血清病毒核酸;腺病毒(+);痰涂片;少量上皮细胞,未发现革兰阳性球菌和革兰阴性杆菌,也没有发现孢子和菌丝。
思维提示:
结合患者病史,与入院即刻检查所提供的结果,诊断社区获得性肺炎明确,经经验性抗感染治疗5天,病情进行性进展。因此,需要考虑何种病原微生物为本患者致病原。而在短时间内能完成的检查项目CT、病毒核酸检查以及痰涂片检查是最为简便和快速的。从以上检断结果能快速告知接诊医师,导致患者治病原因并进行诊欣性治疗。
治疗方案及理由:
1.治疗患者由分诊护士直接送入急诊抢救室,给予心电监护,文丘里面罩吸氧,氧流量10L/min,FiO250%。患者仍憋气,遂给予无创通气( NIPPV),参数IPAP(吸气正压):12cmH2O,EPAP(呼气正压):6cmH2O,FiO260%;坚持半小时,患者不耐受,放弃 NIPPV氧疗。为了给患者提供更好的通气和改善换气,并促进排痰,在争得患者家属同意的前提下,予气管插管机械通气治疗。为了得到更好的护理和监测,将患者收住急诊监护室(EICU)。腺病毒核酸检测阳性,给予广谱抗病毒治疗,停止使用抗革兰阳性和阴性药物。溴环乙胺醇(沐舒坦)积极化痰,同时确保气道湿化,促进气道分泌物排出。给予全身免疫支持治疗,比如胸腺肽1.2μg,肌内注射,每12小时1次。全身营养支持。
2.理由
(1)机械通气治疗:患者发热10天,咳嗽、咳痰伴左侧胸痛,呼吸急骤,频率24次/分,动脉血气分析PaO254.5mmHg(文丘里吸氧10L/min,FiO250%),PaO2/FiO2=109;胸部CT提示左肺大面积实变,右肺渗出性改变。符合重症社区获得性肺炎诊断标准。在给予文丘里以及 NIPPV支持通气的情况下,患者氧合无改善。而且患者咳痰无力,因此选择机械通气。选择机械通气能很好地改善患者通气,加强痰液引流,促进气道分泌物排出,同时给予镇静,能让患者得到很好的休息,减少患者的焦虑。
(2)抗病毒治疗:在社区获得性肺炎中,病毒感染占有相当的比例。在腺病毒核酸检测阳性的情况下,给予针对性治疗是正确选择。但是,由于目前没有针对腺病毒感染的特异性抗病毒药物,于是选择了更昔洛韦广谱抗病毒治疗。
(3)免疫增强治疗:患者为年轻男性,既往体健,本次病毒感染之后病情进展比较凶险,结合住院期间辅助检查T淋巴计数检测提供的结果,考虑存在免疫力下降的情况。因此,选择胸腺肽和丙种球蛋白进行免疫增强治疗,符合该类疾病的治疗原则。
(4)支持治疗:患者进入EICU,接受机械通气之后,包括排痰、全身营养支持等,这些措施均是为患者病情缓解及恢复提供条件。
治疗效果:
1.患者在转诊当天从抢救室转入EICU,接受机械通气支持治疗,并给予镇静措施,以便人机能协调。
2.根据检查结果,采取针对性抗病毒治疗措施和免疫增强措施以及全身营养支持治疗。
3.机械通气之后,呼吸机参数一度给予高强度支持,包括F02最高曾达到80%,PSP达到24cmH2O,PEEP达到10cmH2O,而SpO2也オ仅仅维持在90%左右。随后,上述指标逐渐下降,患者在插管后第7天顺利拔出气管插管,并转入呼吸科普通病房,2周后出院,院外继续观察。
思维提示:
对于社区获得性肺炎,明确病原微生物非常重要。如果在病原微生物不明确的前提下,经经验性抗感染治疗,一部分病例中能取得疗效,但也有一部分病例效果不明显,甚至无效。因此需尽早采取措施,子我感染的原因,或者经验性调整治疗方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
92
#获得性#
80
学习了
107
学习
147
阅读
139
学习
125
学习
131
#社区#
68