Neurology:维生素D、吸烟和EBV可预测多发性硬化症患者长期认知功能
2021-04-17 MedSci原创 MedSci原创
认知障碍是多发性硬化症(MS)常见的衰弱症状,严重影响患者的生活质量。目前尚无理想的治疗方法,亟需可以预防或延缓认知能力下降的有效疗法。低维生素D、吸烟、Epstein-Barr病毒(EBV)核抗原1
认知障碍是多发性硬化症(MS)常见的衰弱症状,严重影响患者的生活质量。目前尚无理想的治疗方法,亟需可以预防或延缓认知能力下降的有效疗法。低维生素D、吸烟、Epstein-Barr病毒(EBV)核抗原1(EBNA-1)抗体升高都是MS发生的危险因素。然而,这些MS风险因素是否可预测患者的长期认知情况尚未清楚。
既往研究中,研究人员曾报道,在临床试验BENEFIT的参与者中,招募后1年或2年时维生素D水平较高者,在5年随访期间活动性病变较少,脑萎缩较少。新的研究中,研究人员将随访时间延长至11年,并考察维生素D、吸烟和抗EBNA-1抗体在复发缓解型MS首次表现后早期是否有助于预测长期的认知功能和神经轴突完整性,研究结果已发表于Neurology。
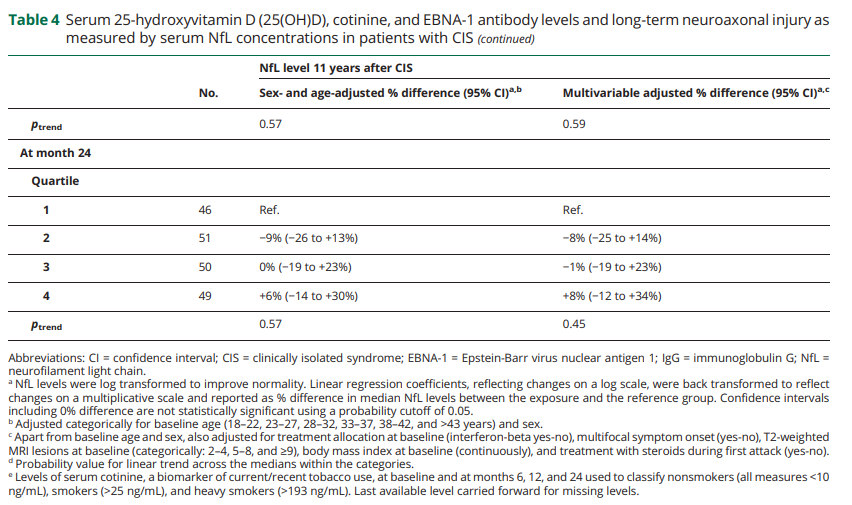
研究纳入278名参加临床试验BENEFIT并完成11年评估(BENEFIT-11)的患者。基线和第6、12和24个月测量了血清25-羟基维生素-D(25(OH)D)、可替宁(吸烟生物标志物)和抗Epstein-Barr病毒核抗原1(EBNA-1)免疫球蛋白G(IgG)的水平,并研究这些生物标志物是否有助于预测11年时Paced听觉序列加试(PASAT)-3评分和血清神经丝轻链(NfL)浓度。使用线性和逻辑回归模型校正性别、基线年龄、治疗分配、类固醇治疗、多灶症状、T2病变和体重指数。
结果显示,更高浓度 的维生素D预测的效果较好, 而吸烟预测认知能力的效果较差。前2年平均25(OH)D升高50-nmol/L与第11年PASAT表现较差的几率降低65%有关(95%置信区间[95%CIs]:0.14-0.89)。吸烟者和重度吸烟者的标准化PASAT评分低于非吸烟者(P趋势=0.026)。基线抗EBNA-1 IgG水平不能预测认知能力(p趋势=0.88)。与第11年NfL浓度的关联证实了这些发现--前2年平均25(OH)D升高50nmol/L与NfL降低20%相关(95% CI:-36%至0%),而吸烟者的NfL水平比不吸烟者高20%(95% CI:2%-40%)。抗EBNA-1抗体与NfL无关。
综上所述,该研究结果表明,临床发病后较低的维生素D和吸烟可预测多发性硬化症患者长期认知功能和神经元完整性的恶化。
原始出处:
Marianna Cortese, et al., Vitamin D, smoking, EBV, and long-term cognitive performance in MS 11-year follow-up of BENEFIT. Neurology. 2020 May 5; 94(18): e1950–e1960. doi: 10.1212/WNL.0000000000009371
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#硬化症#
72
#多发性#
92
#Neurol#
67
#EBV#
87
非常好。
129