Cell:CLP1 突变能引发罕见神经系统疾病
2014-04-28 MedSci MedSci原创
日前,两个独立的研究团队发现,特定基因上的突变会引发一种影响外周和中枢神经系统的新遗传疾病。研究显示,这种突变会干扰 tRNA 的生成,使神经元前体细胞更容易凋亡。这两篇论文于 4 月 24 日发表在Cell杂志上。 研究人员对大量患有神经系统疾病的家庭进行了 DNA 测序,并由此发现了一种以头围减小、感知和运动能力受损为特征的疾病。这种疾病是 CLP1 基因突变引起的,该基
日前,两个独立的研究团队发现,特定基因上的突变会引发一种影响外周和中枢神经系统的新遗传疾病。研究显示,这种突变会干扰 tRNA 的生成,使神经元前体细胞更容易凋亡。这两篇论文于 4 月 24 日发表在Cell杂志上。
研究人员对大量患有神经系统疾病的家庭进行了 DNA 测序,并由此发现了一种以头围减小、感知和运动能力受损为特征的疾病。这种疾病是 CLP1 基因突变引起的,该基因负责调控细胞中的 tRNA 代谢。研究人员认为,解析这一罕见疾病的发病机制,将有助于治疗一些更常见的神经学疾病。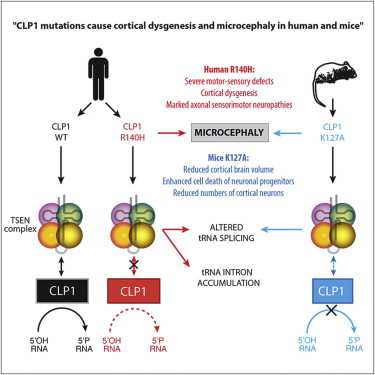
加州大学的 Joseph Gleeson 教授表示:“将这两项研究放在一起我们可以看到,如果完全以患者症状或临床表现来定义疾病,是很难将这种新遗传病区分出来的。在我们明确了致病基因之后,就看到了患者之间的共同特征。这与传统的疾病定义模式完全相反,代表了医学领域的一个转变。”
研究人员发现,携带 CLP1 基因突变的儿童表现出类似的症状,例如大脑畸形、智力障碍、癫痫、感知和运动缺陷等。奥地利科学院的 Josef Penninger 表示:“解析调控神经元退化的基础通路,就可以对其加以调整,在肌萎缩侧索硬化症(ALS)等疾病中保护运动神经元。”
CLP1 蛋白对于 tRNA 的生成非常重要,这种分子负责将氨基酸运送到核糖体,以便装配成为蛋白。人们知道,影响 tRNA 生产的突变与人类神经系统疾病有关,例如脑桥小脑发育不全(PCH)。PCH这是一种目前还无法治愈的儿童神经退行性疾病。
DNA 测序显示,有七个家庭携带同样的 CLP1 突变,而这一突变与运动缺陷、语言障碍、癫痫、脑萎缩和神经元死亡有关。这是首次揭示 CLP1 在人类疾病中的作用。
研究人员发现, CLP1 突变干扰了 tRNA 的生成,使大脑中的神经元前体细胞(或干细胞)更容易凋亡。基因突变让神经元前体细胞(或干细胞)对凋亡通路更为敏感,这是神经生物学领域中的一个新概念。研究人员认为,人们需要重新审视那些可能归入这一范畴的疾病,例如 ALS。
AMC 的 Frank Baas 指出, CLP1 突变引起的疾病是一种新型的PCH。他说:“鉴定这种疾病中的遗传因素,可以帮助我们做出更准确的诊断,为患儿家庭提供更好的帮助。”去年有研究鉴定了一种严重PCH中的基因突变, 并向人们展示一种营养补充剂有望预防或逆转这种疾病。
在去年Nature上,也发表类似文章认为CLP1通过tRNA影响运动神经元的功能。
原始出处:
Ender
Karaca, Stefan Weitzer, Davut Pehlivan, Hiroshi Shiraishi, Tasos
Gogakos, Toshikatsu Hanada, Shalini N. Jhangiani, Wojciech Wiszniewski,
Marjorie Withers, Ian M. Campbell, Serkan Erdin, Sedat Isikay, Luis M.
Franco, Claudia Gonzaga-Jauregui, Tomasz Gambin, Violet Gelowani,
Jill V. Hunter, Gozde Yesil, Erkan Koparir, Sarenur Yilmaz, Miguel
Brown, Daniel Briskin, Markus Hafner, Pavel Morozov, Thalia A. Farazi,
Christian Bernreuther, Markus Glatzel, Siegfried Trattnig, Joachim
Friske, Claudia Kronnerwetter, Matthew N. Bainbridge, Alper Gezdirici,
Mehmet Seven, Donna M. Muzny, Eric Boerwinkle, Mustafa Ozen, Baylor
Hopkins Center for Mendelian Genomics, Tim Clausen, Thomas Tuschl, Adnan
Yuksel, Andreas Hess, Richard A. Gibbs, Javier Martinez, Josef M.
Penninger, James R. Lupski Human CLP1 Mutations Alter tRNA Biogenesis, Affecting Both Peripheral and Central Nervous System Function
PDF (4.6 MB) |
Extended PDF (8.6 MB) |
Download Images(.ppt)|
相关出处:
Hanada T, Weitzer S, Mair B, Bernreuther C, Wainger BJ, Ichida J, Hanada
R, Orthofer M, Cronin SJ, Komnenovic V, Minis A, Sato F, Mimata H,
Yoshimura A, Tamir I, Rainer J, Kofler R, Yaron A, Eggan KC, Woolf CJ,
Glatzel M, Herbst R, Martinez J, Penninger JM.CLP1 links tRNA metabolism to progressive motor-neuron loss.Nature. 2013 Mar 28;495(7442):474-80.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
48
#Cell#
59
#CLP#
79
#神经系统#
67
#罕见#
74