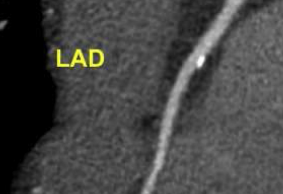
盘点:近期冠状动脉疾病亮点研究一览
2016-09-03 MedSci MedSci原创
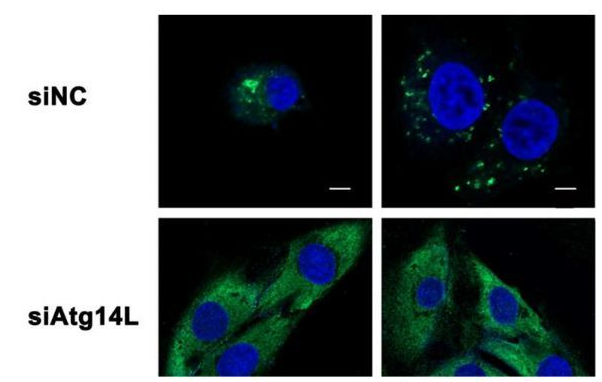
美国食品和药物管理局(FDA)近日批准了首个完全生物可吸收支架用于治疗冠状动脉疾病。这款由雅培(Abbott)开发的支架名为Absorb GT1 BVS(生物可吸收血管支架系统),可释放药物依维莫司(everolimus) 来限制疤痕组织的生长,并且可在大约3年的时间内被人体完全吸收。根据美国国家心肺血液研究所(NHLBI)数据,在美国有1500万人患有冠状动脉疾病,每年由该病导致的死亡病例多

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很好,不错,以后会多学习
75
值得学习
71
值得学习
76
收藏先
80
#冠状动脉疾病#
47
学习了谢谢。
73
学习了,好
56
分享快乐?
55