盘点:黑色素瘤近期重要研究进展汇总
2018-04-21 MedSci MedSci原创
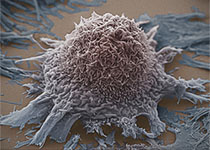
黑色素瘤,又称恶性黑色素瘤,是来源于黑色素细胞的一类恶性肿瘤,常见于皮肤,亦见于黏膜、眼脉络膜等部位。黑色素瘤是皮肤肿瘤中恶性程度最高的瘤种,容易出现远处转移。早期诊断和治疗因而显得尤为重要。这里梅斯小编整理了近期关于黑色素瘤的重要研究进展,与大家一同分享。【1】ipilimumab在NY-ESO-1阳性黑色素瘤患者中的作用免疫检查点抑制剂显著改变了转移性黑色素瘤患者的治疗选择。但是部分患者仍
黑色素瘤,又称恶性黑色素瘤,是来源于黑色素细胞的一类恶性肿瘤,常见于皮肤,亦见于黏膜、眼脉络膜等部位。黑色素瘤是皮肤肿瘤中恶性程度最高的瘤种,容易出现远处转移。早期诊断和治疗因而显得尤为重要。这里梅斯小编整理了近期关于黑色素瘤的重要研究进展,与大家一同分享。
【1】ipilimumab在NY-ESO-1阳性黑色素瘤患者中的作用
免疫检查点抑制剂显著改变了转移性黑色素瘤患者的治疗选择。但是部分患者仍然对治疗没有反应。回顾性数据表明ipilimumab在NY-ESO-1阳性的黑素瘤患者中具有更高的临床益处。25名先前未经治疗或治疗的转移性黑素瘤患者在第1,4,7,10天接受ipilimumab,剂量为10mg / kg,然后进行为期3个月的维持治疗,最长48周。结果表明,疾病控制率为52%。按照RECIST标准,无进展生存期为7.8个月,中位OS为22.7个月,相应的1年生存率为66.8%。治疗相关的3级不良反应事件发生率为36%,无4-5级不良反应事件。 NY-ESO-1特异性细胞或体液免疫应答与临床活动之间没有明确的关联。表明Ipilimumab在这个生物标志物(NY-ESO-1)定义的人群中表现出临床相关的活性。
【2】Selumetinib联合Dacarbazine治疗转移性葡萄膜黑色素瘤
葡萄膜黑色素瘤是最常见的成人原发眼内肿瘤,尚缺乏有效的治疗方案。Selumetinib (AZD6244,ARRY-142886)是一种口服的选择性MEK1/2抑制剂,半衰期短。Ⅱ期临床试验表明其在转移性葡萄膜黑色素瘤患者中具有单药活性。Ⅲ期临床试验纳入的患者为未接受过系统治疗的转移性葡萄膜黑色素瘤患者,患者随机(3:1)分为Selumetinib(75mg 每天2次)联合Dacarbazine(1000mg/m2,21天周期中的第1天静脉输入)或安慰剂联合Dacarbazine。最终纳入129例患者,Selumetinib联合Dacarbazine组中,82例患者出现无进展生存,安慰剂联合Dacarbazine组24例患者出现无进展生存。Selumetinib联合Dacarbazine组客观反应率为3%,安慰剂联合Dacarbazine组为0%。最常见的不良反应为恶心、皮疹、虚弱、腹泻和外周水肿。表明转移性葡萄膜黑色素瘤患者中,Selumetinib联合Dacarbazine具有一定的安全性,但是与安慰剂联合Dacarbazine组相比并未显着改善无进展生存情况。
【3】Keytruda辅助治疗可显著提高III期黑色素瘤患者生存率
PD1抑制剂Keytruda(健痊得)可显著延长晚期黑色素瘤患者的无进展生存期以及总生存期。近日研究人员考察了Keytruda作为辅助治疗手段用于III期可切除高风险黑色素瘤患者的疗效。接受手术的III期黑色素瘤患者每3周随机接受200mg Keytruda或安慰剂,治疗总计18次,约1年时间。共1019名患者参与研究,平均随访15个月,Keytruda可显著延长患者无复发生存期及无复发生存率。在853名PD1表达阳性亚组中,Keytruda组患者1年无复发生存率为77.1%,对照组为62.6%,复发或死亡HR为0.54。14.7%的Keytruda组患者报告3-5级不良事件,对照组为3.4%。Keytruda组发生1例治疗相关的肌炎死亡。表明对于接受手术治疗的III期高风险黑色素瘤患者,200mg Keytruda辅助治疗可显著提高患者无复发生存率。
【4】肥胖可提高部分转移性黑色素瘤患者的总体预后
肥胖与多种癌症的死亡率增高相关;但目前尚不知道肥胖与转移性黑色素瘤的存活预后之间的关系。现研究人员对体重指数(BMI)与进行靶向治疗、免疫治疗或化疗的转移性黑色素瘤患者的无进展存活期或总体存活情况之间的关联进行评估。研究人员对随机参与靶向治疗、免疫治疗或化疗的临床试验的独立队列的和一进行免疫治疗的回顾性研究中的转移性黑色素瘤患者进行回顾性分析,根据BMI将患者划分为体重过轻、正常、超重和肥胖。排除无BMI数据和体重过轻的患者。2006年8月8日-2016年1月15日,共6个队列包含2046名转移性黑色素瘤患者,1918位患者被纳入本次分析,接受靶向治疗、免疫治疗或化疗分别有839人、538人和541人。结果表明,对于转移性黑色素瘤患者,肥胖可相对正常BMI延长其无进展存活期和整体存活率,这一关联主要见于采取靶向治疗或免疫治疗的男性患者。
【5】NF1突变与结膜黑色素瘤发生之间的关系
结膜黑色素瘤是潜在致命的眼部肿瘤。尽管局部治疗有效,但肿瘤复发和转移仍然频繁。结膜黑色素瘤的遗传学机制尚未完全明确。近日,研究人员通过靶向的下一代测序筛查了63例结膜黑素瘤患者已知的其它黑素瘤亚型重要的基因突变,评估了突变状态与患者预后之间的关系。结果发现激活MAP激酶途径的基因在结膜黑素瘤患者中存在频繁的突变。NF1突变最为常见(n=21,33%)。复发激活突变也确定了BRAF(n=16,25%)和RAS(n=12,19%; 11个NRAS和1个KRAS)基因。表明结膜黑素瘤可以根据遗传突变分为四组:BRAF突变、RAS突变、NF1突变和三种野生型黑素瘤。该遗传分类有助于评估转移性结膜黑色素瘤患者的治疗选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#色素#
48
#研究进展#
0
#黑色素#
47
#黑色素#
44
了解一下.谢谢分享!
70
一起学习学习
73