AJRCCM: 2022年国内首篇-肺动脉高压患者的认知功能障碍
2022-08-01 刘少飞 MedSci原创
肺动脉高压(PH)是由多种病因引起的肺血管压力逐渐增加的综合征。据报道,PH患者还伴有炎症和脑血流动力学调节受损。然而,这些患者是否存在认知障碍仍不确定。

肺动脉高压(PH)是由多种病因引起的肺血管压力逐渐增加的综合征。其特征是进行性呼吸急促、疲劳和生活质量下降,如运动不耐受、睡眠障碍、焦虑和抑郁。越来越多的证据表明,一些慢性心肺部疾病与炎症、氧化应激和线粒体功能障碍导致的认知障碍有关。据报道,PH患者还伴有炎症和脑血流动力学调节受损。然而,这些患者是否存在认知障碍仍不确定。
针对上述问题,上海市肺科医院肺循环科袁平副研究员和黎金玲主任护师在 同济大学郑加麟教授和夏骁寰研究员指导下,使用简易精神状态检查(MMSE)和蒙特利尔认知评估(MoCA)问卷分析了上海市肺科医院肺循环科收治315例PH患者和315例对照者的认知障碍表现,及认知功能功能障碍与发病风险、严重程度和临床恶化事件之间的关系。结果提示PH患者存在认知障碍,也预疾病的严重程度有关,较低的MMSE和MoCA总评分能独立预测发病风险增加和预后较差等表现。该研究工作首次发现了肺动脉高压疾病进展与神经认知功能变化间的关系,提出了肺脑轴复杂双向互作的重要理念,为肺动脉高压疾病诊断与治疗提供了新的靶标,并提示肺动脉高压患者认知功能异常早期诊断与干预的重要性。上述研究成果于7月29日在线发表于国际权威刊物American Journal of Respiratory and Critical Care Medicine(论文的第一作者为上海市肺科医院肺循环科袁平副研究员和黎金玲主任护师,通讯作者为郑加麟教授、夏骁寰研究员)。
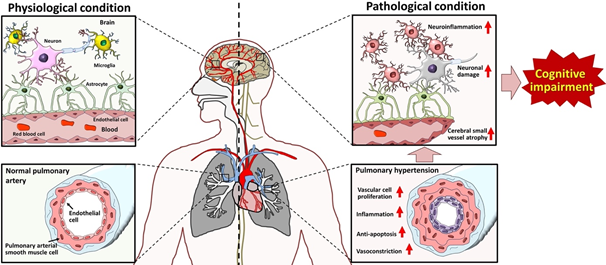
图1 肺动脉高压患者认知功能障碍。
参考文献:
Ping Yuan, Jinling Li, Jianhui Liu, Hongting Liu, Sugang Gong, Lan Wang, Jinming Liu, Congcong Li, Yi Wang, Xiaohuan Xia, and Jialin C. Zheng. Cognitive dysfunction in patients with pulmonary hypertension. Am J Respir Crit Care Med. 2022 Jul 29. doi: 10.1164/rccm.202204-0726LE. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#RCC#
101
#动脉高压#
140
#肺动脉高压患者#
171
#功能障碍#
126