单绒毛膜双羊膜囊双胎之间隔膜破裂致羊膜带综合征2例
2018-03-24 佚名 实用妇产科杂志
患者,26岁,因孕25周,发现双胎之一畸形3+月于2013年10月11日收入中山大学附属第一医院。
例1
【一般资料】
患者,26岁,
【主诉】
因孕25周,发现双胎之一畸形3+月于2013年10月11日收入中山大学附属第一医院。
【个人史】
患者为自然受孕,G1P0。
【现病史】
早孕期无放射性物质、毒物接触史,平时当地医院定期产检。孕6周超声检查示:官内1个妊娠囊,可见胚芽及胎心搏动,宫内单胎妊娠6周。孕1l+2周,超声检查发现单绒毛膜双羊膜囊(monochorionicdiamniotictwins,MCDA)双胎,胎儿顶臀长分别相当于ll/11周。孕13周,超声检查发现MCDA双胎,胎儿顶臀长分别相当于13/13周,其中一胎儿脑膨出。孕14+2周转诊至中山大学附属第一医院,超声检查结果显示单绒毛膜单羊膜囊(monochorionicmonoamniotictwins,Mc.MA)双胎,其中一胎颅骨环未显示,脑组织连于胎膜上,考虑羊膜带综合征。患者及家属选择继续妊娠,于孕17周行产前诊断,羊水染色体检查结果为正常核型,染色体微阵列分析(cMA)未发现异常。经过详细遗传咨询,患者及家属要求行选择性减胎术减灭畸形胎儿,于孕25周收入院。
【体格检查】
生命体征平稳,多普勒超声检查可探及2个胎心,
【辅助检查】
入院后血常规、凝血功能及血液生化均未见异常。
【治疗】
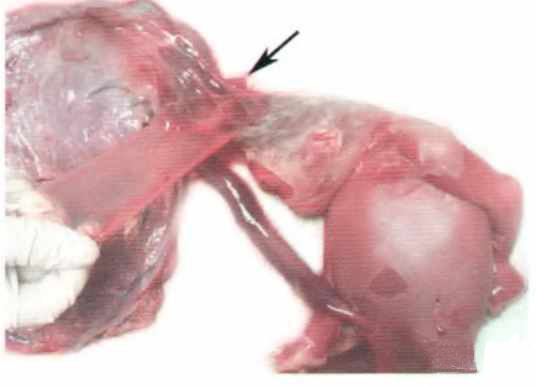
孕25+3周行超声引导下射频消融减胎术,术毕超声监测显示畸形胎儿心搏停止,保留胎儿胎心正常。减胎术后第2天患者自觉胎动消失,复查超声显示保留胎儿死亡。引产后见被减胎儿胎体充血,颅骨缺损,脑组织连于胎膜上,唇腭裂;保留胎儿胎体较苍白,外观未见畸形(见图l、图2);胎盘为1个,胎盘上可见残留的双羊膜囊双胎之间的隔膜,两胎儿的脐带插入胎盘部位分别位于隔膜两侧。病理解剖发现被减胎儿两条脐动脉已凝固,脐静脉入肝段未完全凝固。患者引产后恢复良好。

例2
【一般资料】
患者,28岁
【主诉】
因孕26周,发现双胎之一宫内死亡1天于2013年4月22日收入中山大学附属第一医院。
【个人史】
患者为自然受孕,平素无规律产检。
【现病史】
孕8周、13周当地医院超声检查均显示为McDA双胎,胎儿存活,大小与孕周数相符。患者未行唐氏筛查及其他孕期检查,孕23周当地医院超声检查发现两胎儿均相当于22周,胎儿之间的隔膜消失,两胎儿位于同一羊膜腔内,脐带插入胎盘处有异常回声包裹,建议其转上级医院诊治。孕26周患者到中山大学附属第一医院就诊,行超声检查发现McMA双胎,其中一胎儿死亡,颅骨塌陷变形,发育相当于23周;存活胎儿相当于25周;两胎儿脐带在进入胎盘处相互缠绕,存活胎儿脐静脉在缠绕后呈瘤样扩张。经过详细遗传咨询,患者及家属担心幸存胎儿神经系统损伤,要求终止妊娠,故收入院。患者G2P1,3年前顺产一女婴,体健,否认孕期放射性物质、毒物接触史。
【体格检查】
生命体征平稳,多普勒仅闻及1个胎心音,
【辅助检查】
入院后血常规、凝血功能及血液生化均未见异常,
【治疗】
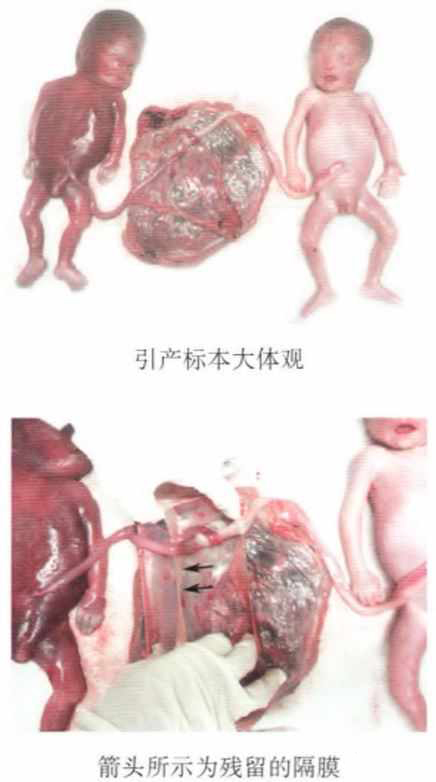
患者及家属拒绝行产前诊断,行羊膜腔穿刺引产。引产后见胎儿1胎体充血,已浸软变形,胎儿2左腕部可见环形羊膜带,宽度O.5cm,松解后羊膜带后腕部见窄缩环(见图3)。检查胎盘为一个,胎盘上可见残留的双羊膜囊双胎之间的隔膜,两胎儿的脐带插入胎盘部位分别位于隔膜两侧,两胎儿的脐带缠绕呈绞索状,胎儿l脐带缠绕段可见缩窄,表面未见羊膜带附着(见图4)。患者引产后恢复良好。

【讨论】
McDA双胎之间的隔膜由两层羊膜组成,由于隔膜破裂、原先分别位于两个羊膜腔内的胎儿处于同一羊膜腔内现象称为假性单羊膜囊双胎(pseud0一monoalllnioticpregnancy),是少见的McDA双胎并发症,1991年至今国内外文献仅有四十余例报道。。羊膜带综合征发生率1/15000—1/1200,是一种由纤维带导致的胎儿先天畸形,其临床表现多样,从肢体末端窄缩环、截肢到颅面部畸形甚至胸腹壁缺损均有报道。1965年Torpin提出了羊膜破裂致畸理论,即羊膜囊破裂使胎儿和羊水进入绒毛膜腔,羊膜与绒毛膜分离,羊膜的中胚层面和裸露的绒毛膜产生纤维带粘连、缠绕胎儿,导致胎儿畸形。McDA双胎由于隔膜破裂导致羊膜带综合征更为罕见,目前仅有4例病案报道。McDA双胎之间隔膜破裂的原因目前尚不清楚,国内外报道的病例中约有50%(2l/43)有产前诊断或激光、胎儿镜、羊水减量治疗病史,推测羊膜腔侵入性检查及治疗是隔膜破裂的高危因素。本文2例患者在孕期均无上述因素,为隔膜自发性破裂,可能与羊膜发育缺陷、局部薄弱有关。以往McDA双胎之间隔膜破裂主要是由产后检查胎盘发现,本文2例能在产前得到诊断,得益于近年来超声技术的发展和对双胎绒毛膜性、羊膜性的重视。2例患者在早孕期已经超声确定为MCDA双胎,后续超声检查却发现MCMA双胎的表现:如两胎儿之间无羊膜分隔、脐带缠绕。这也是目前国际上产前诊断假性单羊膜囊双胎的依据。羊膜带综合征的严重程度和影响范围取决于羊膜囊破裂的时间、位置以及胎体被羊膜带粘连缠绕的部位。病例1孕11+2周超声检查尚未发现异常,孕13周超声发现隔膜消失和典型的羊膜带综合征超声表现。而病例2孕13周尚未发现异常,孕23周超声发现隔膜消失但未见典型羊膜带综合征的表现,引产后才发现胎儿肢体被羊膜带缠绕。可能表明隔膜破裂出现的孕周越早,羊膜带粘连的位置越广,病变以组织缺损为主;中晚孕发生隔膜破裂的病例羊膜带可缠绕、压迫、勒紧肢体或脐带,造成肢体窄缩环、截肢甚至宫内死胎,但当羊膜带与胎儿粘连的部位少、位置隐蔽或两胎儿相互遮挡可能造成产前漏诊。此外,将羊膜带误认为双胎羊膜形成的隔膜一1或隔膜不完全破裂、残存的隔膜掩盖了羊膜带的声像也可能导致漏诊。隔膜和羊膜带超声声像均表现为漂浮在羊水中的纤细强回声光带,但隔膜不与胎儿粘连,而羊膜带与胎体粘连,并可造成胎儿肢体畸形或限制胎儿活动。McDA双胎隔膜破裂除导致羊膜带综合征外,还因两胎儿位于同一羊膜腔内、脐带缠绕的几率显著增加,宫内死胎风险上升。病例2一胎宫内死亡正是由于脐带缠绕过紧、脐血流中断所致,并非由羊膜带综合征直接导致。McDA双胎隔膜破裂所致羊膜带综合征的治疗方案需要综合考虑胎儿的受累程度、胎儿官内情况、治疗操作的可行性以及医学伦理学等因素。对于胎儿未受累或仅轻度受累而孕妇及家属愿意接受者,可按单羊膜囊双胎进行严密监护,适时终止妊娠,产后切除羊膜带。国外有研究尝试在羊膜带缠绕造成截肢畸形前行胎儿镜下羊膜带松解术,但有早产、流产、再次粘连等风险。随着胎儿镜、超声介导射频消融等胎儿官内治疗技术的成熟,选择性减胎有可能成为一胎严重畸形而另一胎儿未受累病例治疗的新方向。病例1患者孕25+3周选择接受超声介导射频消融减胎,但术后保留胎儿死亡。结合病史及解剖结果,考虑孕周超过25周,被减胎儿脐血管较粗,脐静脉未完全凝固,减胎时虽然被减胎儿心搏停止,但保留胎儿通过胎盘吻合血管向被减胎儿失血,最终死亡。孙路明等旧。也报道,孕周超过25周时射频消融减胎手术难度增加。经过近年来的经验总结,我们认为射频消融减胎术前详细评估胎位、胎盘位置、进针方向和深度,争取孕17~23周减胎,或孕25周后减胎时增加凝固血管的时间及循环数有利于保证血管凝固的效果、降低保留胎儿失血和官内死亡的风险。对于一胎官内死亡者,幸存胎儿受累程度及死胎发生时间均需考虑。早孕期一胎死亡,因胎盘吻合血管小,血流变化对幸存胎儿的影响小,如幸存胎儿未受羊膜带影响,可在监护母亲凝血功能的情况下继续妊娠。中晚孕一胎死亡,幸存胎儿会通过胎盘血管吻合向死亡胎儿急性输血,导致幸存胎儿失血性休克、脑损伤。如病例2,中孕期一胎死亡时间接近3周,幸存胎儿可能已发生缺血性脑损伤,但因幸存胎儿有自身代偿恢复,入院时脐血检查无法反映死胎当时的失血和贫血状态,增加预后评估的困难。McDA双胎隔膜破裂所致羊膜带综合征是一种复杂的双胎妊娠并发症,发生率极低,但可能出现羊膜带综合征造成胎儿畸形以及脐带缠绕使胎儿宫内死亡风险显著增高。这2例病例提醒我们在今后的临床工作中,早孕期诊断为McDA双胎如后续检查提示McMA,应警惕隔膜破裂的可能,进行详细的超声检查有无羊膜带、胎儿结构畸形及双胎的脐带缠绕;但由于超声表现多样复杂,部分病例可能漏诊;其治疗策略制订需综合考虑多方因素,详细的遗传咨询和充分的知情选择是非常必要的;选择性减胎有望成为保留未受累胎儿的选择。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#隔膜破裂#
30
好好学习天天向上感谢感谢
64
#综合征#
32
阅
62
典型病例.学习了.
56