Nat Methods:新型人工胸腺可源源不断通过血液干细胞制造大量抗癌T细胞
2017-04-06 生物谷 生物谷
最近,一项发表在国际杂志Nature Methods上的研究报告中,来自加州大学洛杉矶分校(ULCA)的研究人员通过研究开发了一种新系统来制造人类T细胞,T细胞是一种能够帮助机体抵御诱发疾病的外来入侵者的关键白细胞。研究者表示,这种系统能够用来工程化设计T细胞,并且帮助寻找和攻击癌细胞,这就意
最近,一项发表在国际杂志Nature Methods上的研究报告中,来自加州大学洛杉矶分校(ULCA)的研究人员通过研究开发了一种新系统来制造人类T细胞,T细胞是一种能够帮助机体抵御诱发疾病的外来入侵者的关键白细胞。研究者表示,这种系统能够用来工程化设计T细胞,并且帮助寻找和攻击癌细胞,这就意味着,研究人员未来或许有望持续获得T细胞的供给来帮助治疗多种癌症类型。
胸腺位于心脏前面,其在机体免疫系统的功能发挥上扮演着关键角色,通常情况下胸腺能够利用血液干细胞来制造T细胞,从而帮助机体抵御感染,同时清除癌细胞;然而随着年龄增长或者生病等状况,胸腺会慢慢变得不能够对T细胞进行有效制造。胸腺中产生的T细胞能够获得一种名为感受器的特殊受体分子,这些受体分子能够帮助T细胞寻找并且破坏病毒感染的细胞或癌细胞。利用这一过程研究者或许就能够在癌症研究领域进行更为深入的研究,如今科学家们发现,利用特殊靶向癌症的受体来装备大量的T细胞,即过继性T细胞免疫疗法或许就能够在临床试验中表现出出色的结果。
过继性的T细胞免疫疗法通常涉及从癌症患者机体中收集T细胞,利用靶向癌细胞的受体分子在实验室对T细胞进行工程化操作,随后将这些细胞在输送回患者机体中。然而这种疗法往往非常耗时,而且癌症患者机体中通常并没有足够的T细胞来帮助这项疗法的进行。2006年过继性的T细胞免疫疗法首次进入临床试验阶段,科学家们发现,这种疗法能够利用来自供体的血细胞或多能干细胞有效地制造T细胞(提供一个可靠稳定的T细胞来源),然而这种策略所面临的挑战就是,其所制造的T细胞所携带的受体往往并不能同每一个患者进行匹配,最终就会导致患者机体排斥所移植的细胞,并且促进T细胞攻击除了癌细胞以外的健康组织。
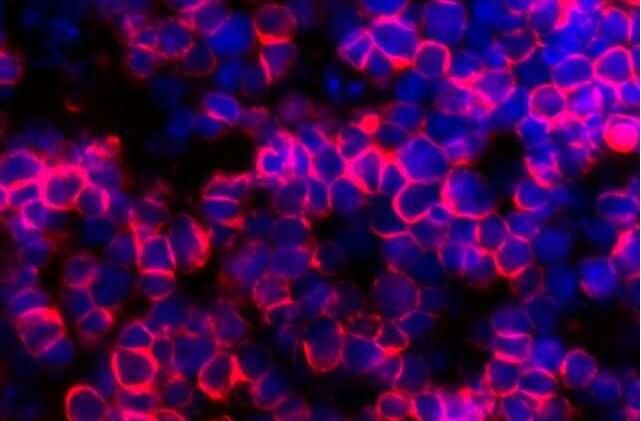
研究者Gay Crooks说道,我们知道,制造持续安全的抗癌T细胞的关键就是利用特殊的方法来控制好整个过程,这种方法就会使得所移植的细胞中的所有T细胞受体失活(除了抵御癌细胞以外的受体)。这项研究中,研究人员利用了多组分组合开发出了一种名为人工胸腺类器官的结构,这种结构类似于机体胸腺,其能够通过血液干细胞来产生T细胞;而且研究者还发现,利用这种人工胸腺类器官开发出的成熟T细胞能够携带多种类型的T细胞受体,而且其工作原理同正常胸腺所产生的的T细胞非常相似。
下一步研究者将会检测是否这种人工胸腺类器官能够产生携带抵御癌症的T细胞受体的特殊T细胞。当研究者将一种能够运输抗癌受体的基因插入到血液干细胞中时,他们发现,这种胸腺类器官能够产生大量的癌症特异性T细胞,而且所有其它的T细胞受体的功能都会被关闭,相关研究结果表明,这些细胞或许就能够被潜在用来抵御癌症,同时还不会带来任何攻击机体健康组织的风险。
最后研究者Montel-Hagen表示,其他从事T细胞开发研究的科学家们或许也能够轻松制造出这种人工胸腺类器官,如今我们正在深入研究如何利用多能干细胞来进行更为深入的研究,多能干细胞能够带来抗癌T细胞的持续稳定供应,从而满足患者在紧急情况下的需求来挽救患者的生命。
原始出处:
Christopher S Seet, Chongbin He, Michael T Bethune, et al. Generation of mature T cells from human hematopoietic stem and progenitor cells in artificial thymic organoids. Nature Methods (2017) doi:10.1038/nmeth.4237.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血液干细胞#
86
#Nat#
69
#MET#
66
#胸腺#
70