JASN:CKD患者肾脏功能下降斜率及其与死亡率和心血管疾病之间的关系
2020-10-12 MedSci原创 MedSci原创
在中度至重度CKD人群中,研究人员观察到eGFR的急剧下降与死亡和心血管事件的风险逐渐增加有关。但是,研究人员没有发现与eGFR改善相关的风险增加。
估计的肾小球滤过率(eGFR)下降斜率与升高的死亡和心血管事件风险呈U形关系。eGFR升高的个体预后不良可能归因于肌肉减少症,血液稀释和其他临床恶化的指标。
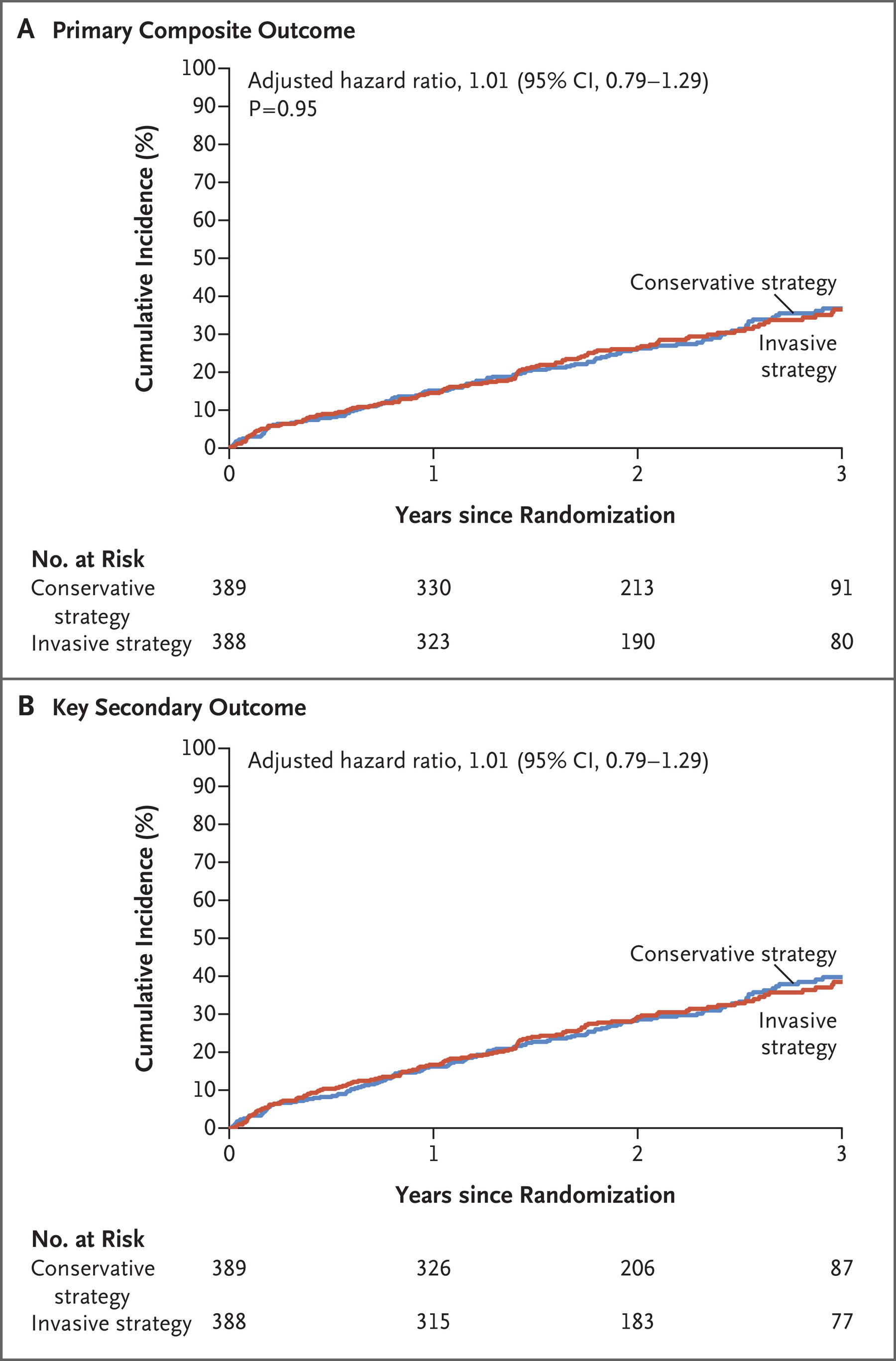
近日,肾脏病领域权威杂志Journal of the American Society of Nephrology上发表一篇研究文章,该研究旨在探究eGFR斜率与死亡或心血管事件风险之间的关联,并考虑多种混杂因素。研究人员分析了2738名中度至重度CKD患者,并使用线性、混合效应模型评估了每年四次eGFR评估的斜率,而采用Cox比例风险模型评估斜率与死亡和心血管事件风险之间的关联。
eGFR斜率呈钟形分布(平均[SD]为每1.73 m2每年-1.5 [-2] ml/min)。eGFR下降幅度大于平均下降幅度,这与死亡(风险比[HR]为1.23;95%置信区间[95%CI]为1.09至1.39)和心血管事件(HR为1.19;95%CI为1.03至1.38)风险的逐步增加相关。eGFR的升高或下降低于平均下降水平与死亡或心血管事件的风险无关。
在中度至重度CKD人群中,研究人员观察到eGFR的急剧下降与死亡和心血管事件的风险逐渐增加有关。但是,研究人员没有发现与eGFR改善相关的风险增加。这些结果支持eGFR斜率在CKD患者临床评估中的潜在价值。
原始出处:
Paula F. Orlandi,et al.Slope of Kidney Function and Its Association with Longitudinal Mortality and Cardiovascular Disease among Individuals with CKD.JASN,2020.https://jasn.asnjournals.org/content/early/2020/10/09/ASN.2020040476
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASN#
89
#CKD患者#
95
#血管疾病#
68
学习学习
141
学习
137