Cell Biol Toxicol:DNA甲基化抑制剂RG108可预防噪音引起的听力损失
2021-04-09 AlexYang MedSci原创
噪音引起的听力损失是一种常见的听力残疾类型,严重影响个人的生活质量。
噪音引起的听力损失是一种常见的听力残疾类型,严重影响个人的生活质量。
最近, 有研究人员评估了DNA甲基化对噪音诱导的听力损失的影响。

研究人员使用选择性抑制剂RG108阻断DNA甲基转移酶1(DNMT1)的活性,或用siRNA沉默DNMT1。在基线和创伤后2天测量了小鼠的听觉脑干反应来评估听觉功能。研究人员还对小鼠内耳样本进行全包埋免疫荧光染色和共聚焦显微镜检查,分析噪音引起的耳蜗和听神经在噪音暴露后2天的损伤。
研究结果发现,噪音暴露引起听觉脑干反应阈值升高和耳蜗毛细胞损失。全包埋耳蜗染色显示内毛细胞和螺旋神经节神经元之间的听觉带状突触密度降低。通过非核苷类特异性药理抑制剂RG108抑制DNA甲基转移酶活性,或用siRNA沉默DNA甲基转移酶-1,可显著减轻ABR阈值升高、毛细胞损伤和听觉突触的损失。

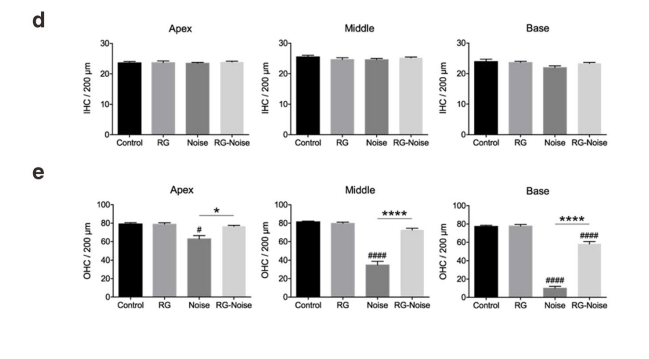
噪音暴露2天后毛细胞(HC)损失和ABR阈值变化评估
最后,研究人员指出,抑制DNMT1可以改善噪音引起的听力损失,表明了DNMT1可能是一个有前景的治疗靶标。
原始出处:
Zhiwei Zheng , Shan Zeng , Chang Liu et al. The DNA methylation inhibitor RG108 protects against noise-induced hearing loss. Cell Biol Toxicol. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
66
#CEL#
70
#Cell#
65
#Biol#
91
#Bio#
69
#听力#
60
感谢好文!
107