四个关键要点,帮你轻松搞定肘关节脱位!
2021-09-27 骨殇 好医术
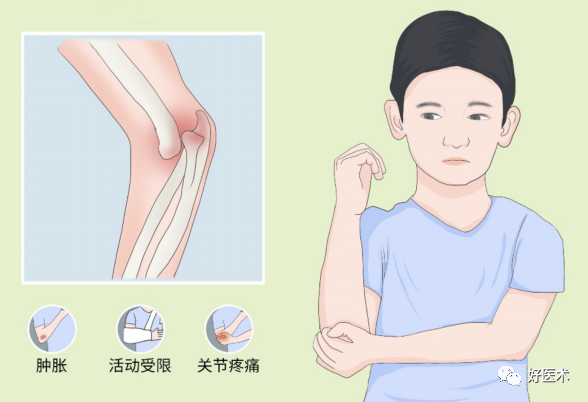
肘关节脱位是肘部常见损伤,多发于青少年,常合并其他损伤,在诊治中应提高警惕,防止漏诊漏治。那么肘关节脱位到底该如何诊疗呢?今天的早读将全面讲解,值得学习借鉴!
肘关节脱位是肘部常见损伤,多发于青少年,常合并其他损伤,在诊治中应提高警惕,防止漏诊漏治。那么肘关节脱位到底该如何诊疗呢?今天的早读将全面讲解,值得学习借鉴!
损伤机制及分类
肘关节脱位多由间接暴力引起,常发生在坠落时上肢外展着地时,是由剪切力造成的。大多数脱位为后脱位。近尺桡关节向后移位时造成桡骨头骨折、桡骨颈骨折和(或)尺骨喙突骨折,外翻的应力还可造成肱骨内上髁的撕脱骨折。
脱位机制示意图

肘关节脱位分类如下
(1)肘关节后脱位
最常见的一型,表现为尺骨鹰嘴向后移位,肱骨远端向前移位的肘关节脱位。
(2)肘关节前脱位
较少见的一型,常合并尺骨嘴骨折,表现为尺骨鹰嘴骨折和尺骨近端向前移位。
(3)肘关节侧位脱位
常见于青少年,暴力致肘关节侧副带和关节囊撕裂,肱骨远端向尺侧或桡侧移位,常伴内或外上髁撕脱骨折。
(4)关节分裂脱位
极少见的一型,表现为尺骨鹰嘴向后脱位,而桡骨小头向前移位,肱骨远端便嵌插在二骨端之间。
临床表现及诊断
明确外伤史,肘关节肿胀,肘关节呈半屈曲状,伸屈功能障碍,肘后三角形骨性标志紊乱。
正常肘后三角关系
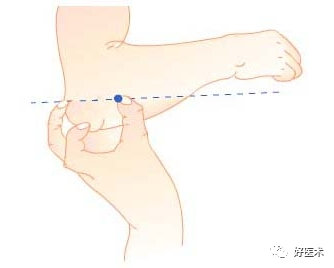
肘后三角关系紊乱

如为肘关节后脱位,尺骨鹰嘴向后明显突出,肘关节后方空虚。如为肘关节侧方脱位,肘关节呈内或外翻畸形。X线可以明确诊断。需注意仔细检查上肢的神经、血管功能。
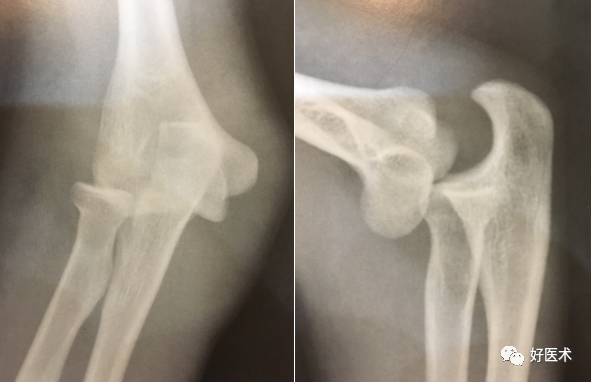
(1)肘关节后脱位
后脱位表现为肘关节呈屈肘45°位置,肘部疼痛、肿胀、畸形、关节活动明显受限,肘后三角关系失常。
1)正位片显示桡、尺骨上端与肱骨下端相重叠,正常肘关节间隙消失;
2)侧位片显示桡骨头和尺骨鹰嘴向后上方移位,肱骨下端则移向前下方,尺骨喙突常居于肱骨鹰嘴窝内;
3)除肘关节后脱位外,常同时伴有桡、尺骨向外或向内移位;
4)常合并桡骨头、尺骨喙突、肱骨内上髁及肱骨外髁等骨折。
右肘关节后脱位:右肘关节位置关系失常,右桡骨头和尺骨鹰嘴向后上外方移位
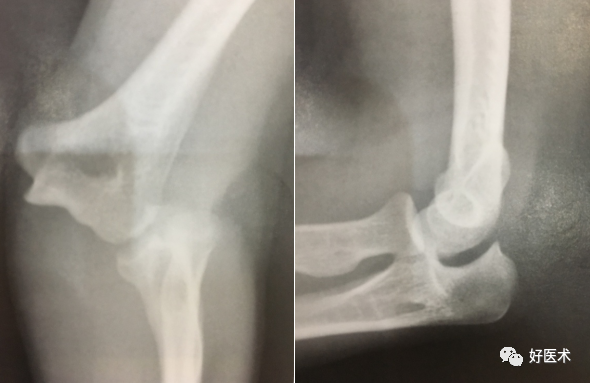
左肘关节后脱位并桡骨头骨折:左桡、尺骨上端相对肱骨下端向后外上方移位,同时桡骨头粉碎性骨折

(2)肘关节前脱位
前脱位肘关节常处于伸直位,肘后可触及肱骨远端嘴窝,肘后空虚,肘后三角正常关系丧失。
1)侧位片见尺、桡骨脱位至肱骨下端之前方;
2)多数伴尺骨嘴的粉碎性骨折。

(3)肘关节侧方脱位
侧方脱位肱骨远端侧方可触及尺骨嘴,伸屈活动受限,有内收外展的异常活动。
1)正位片可见肘关节呈明显的外翻畸形,尺、桡骨向外方移位;
2)侧位片仅见肱骨髁与尺、桡骨重叠,无前、后脱位现象;
3)偶可合并尺骨半月切迹或肱骨外髁骨折。
左肘关节侧方脱位:左肘关节关系失常,桡、尺骨上端相对肱骨下端向外侧方移位
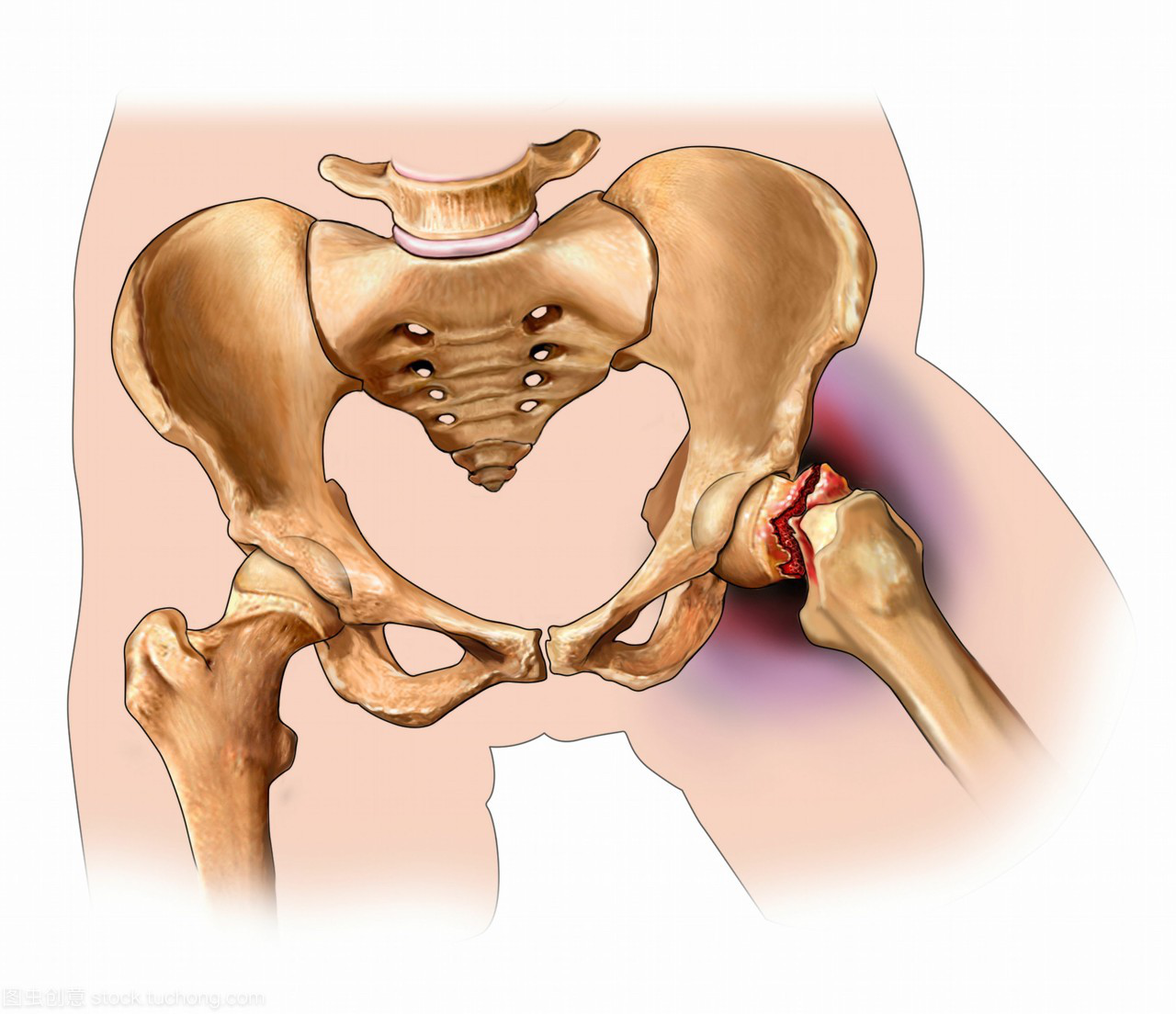
并发症
(1)肱动脉损伤
在肘关节脱位时肱动脉损伤是严重的并发症,较为见。血管受到牵拉造成内膜撕裂以致断裂,早期诊断非常重要。如果闭合复位后动脉循环未恢复,则需立即进行动脉修复,通常要用大隐静脉移植修复动脉缺损。如果延迟进行手术治疗,需要切开前臂筋膜防止筋膜间隙综合征的发生。内膜撕裂可导致动脉迟发的血栓形成,肘关节脱位复位后要密切观察患肢循环。
(2)筋膜间室综合征
复位后通常有严重肿胀,需严密观测防止筋膜间室综合征的发生。
(3)神经损伤
肘关节脱位时可造成神经损伤,多为牵拉伤,经保守治疗可恢复其功能。
(4)肘关节不稳
肘关节反复脱位造成肘关节周围组织愈合不良、韧带松弛或复位而未能修复损伤的侧副韧带时可导致肘关节不稳。需手术修复侧副韧带。
肘关节脱位时,进行尺神经、正中神经和肱动脉损伤相应检查
治 疗
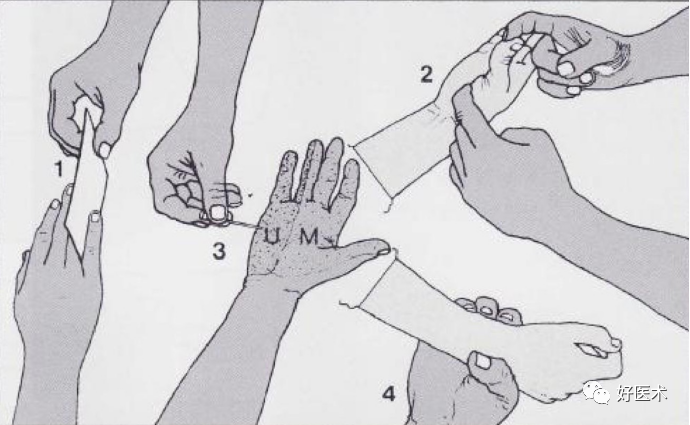
(一)手法复位
新鲜肘关节脱位或合并骨折的脱位主要治疗方法为手法复位,石膏托固定3周。麻醉下取坐位进行牵引与反牵引,将肘关节屈曲60°~90°,并可稍加旋前,常有复位感。合并骨折时,先复位关节,再复位骨折。超过3周的陈旧性脱位亦可试行手法复位,固定时肘关节要<90°。
肘关节脱位手法复位

(二)手术治疗
(1)适应证:
1)闭合复位失败或不宜进行闭合复位;
2)合并骨折时,关节复位后骨折不能复位;
3)陈旧性脱位,不宜进行手法复位者;
4)某些习惯性肘关节脱位。
(2)开放复位:取肘关节后侧路,保护尺神经,为防止再脱位,用一枚克氏针固定肘关节1~2周。
(3)关节形成术:适用于肘关节陈旧性脱位、软骨面已经破坏或肘关节已强直者。
(三)复杂性肘关节骨折脱位及其治疗
(1)肘关节脱位合并桡骨小头或肱骨小头骨折:手法复位肘关节,如果桡骨小头骨折无移位或复位成功,上肢石膏固定3周。如果桡骨小头粉碎骨折或复位失败,则手术切除桡骨小头;
(2)肘关节脱位合并桡骨干骨折:手法复位效果较满意。肘关节复位后,如果桡骨干骨折再经手法复位成功,则上肢石膏固定4~6周。如果桡骨干骨折复位失败,则手术复位内固定;
(3)肘关节脱位合并肱骨外髁、桡骨颈骨折:采用手法复位,如果肱骨外髁外翻90°,则不能用牵引方法复位肘关节;如果肱骨外髁、桡骨颈骨折复位成功,则上肢石膏固定4~6周;如果肱骨外髁、桡骨颈骨折复位失败,则采用手术复位;
(4)肘关节侧方脱位合并脓骨外髁骨折:如果肱骨外髁无外翻,应手法复位,避免牵引,将肘关节稍屈曲并稍内翻,用鱼际推按尺桡骨近端及外髁骨折块即可复位。如果外髁骨折块未复位,再试用手法复位。如果肱骨外复位失败,则采用手术复位;
(5)肘关节脱位合并上尺桡关节分离及肱骨外骨折:该损伤较复杂,可行手法复位;
(6)肘关节伸展性半脱位:该损伤少见,因此易于误诊和漏诊。有跌倒手掌着地外伤史,肘关节疼痛、肿胀,肘关节呈超伸展位僵直,不能屈曲活动,伸屈功能障碍线可以发现肱骨滑车向掌侧明显突出并外旋,尺骨明显后伸,尺骨、肱骨干呈-20°~35°角,鹰嘴关节面离开了与滑车关节面的正常对合关系。牵引下屈曲肘关节即可复位,上肢石膏固定3周。
参考文献:
[1]Kim Jin Young,Choi Guk Jin. Lateral Elbow Dislocation of a Patient with Elbow Flexion Contracture and a Traumatic Brain Lesion.[J]. The journal of hand surgery Asian-Pacific volume,2021,26(3):
[2]公茂琪,蒋协远.对肘关节后脱位、肘关节后外侧旋转损伤及肘关节恐怖三联征内在联系的思考[J].骨科临床与研究杂志,2020,5(02):65-67.
[3]Dimantha W H D,Pathinathan Kalaventhan,Sivakumaran Dishanth,Gunawardena P M P,Madushanger S R,Wijesinghe Sunil. Pediatric anterior elbow dislocation due to a rare mechanism of injury: A case report.[J]. International journal of surgery case reports,2021,85.
[4]孙伟桐,蒋协远,公茂琪,查晔军.不同类型肘关节损伤冠状突骨折特点研究进展[J].中华肩肘外科电子杂志,2018,6(04):307-312.
[5]孙伟桐,蒋协远,公茂琪,查晔军.陈旧性肘关节脱位的诊断与治疗[J].国际外科学杂志,2020,47(11):721-725.
[6]Hoyt W. Benjamin,Clark M. DesRaj,Walsh A. Sarah,Pensy A. Raymond. Surgical Elbow Dislocation: Technique and Comparative Outcomes[J]. Techniques in Orthopaedics,2021:
[7]Nima Rezaie,Sunny Gupta,Benjamin C. Service,Daryl C. Osbahr. Elbow Dislocation[J]. Clinics in Sports Medicine,2020,39(3):
声明:本文为原创内容,作者骨殇老师,仅用于学习交流,未经授权禁止转载!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#关节脱位#
0
#肘关节#
97
#肘关节脱位#
88
#脱位#
105
学习了
102
学习了
99
xuedaole
101