IJBCB:乙酰胆碱酯参与帕金森疾病模型中多巴胺能神经元的凋亡过程
2013-01-09 IJBCB SIBS
2012年12月21日,国际学术期刊International Journal of Biochemistry and Cell Biology在线发表了 生化与细胞所张学军研究组的最新研究成果—“Acetylcholinesterase deficiency decreases apoptosis in dopaminergic neurons in the neurotoxin model o
2012年12月21日,国际学术期刊International Journal of Biochemistry and Cell Biology在线发表了 生化与细胞所张学军研究组的最新研究成果—“Acetylcholinesterase deficiency decreases apoptosis in dopaminergic neurons in the neurotoxin model of Parkinson’s disease”。该研究不仅证实了乙酰胆碱酯酶Acetylcholinesterase(AChE)确实参与到了帕金森疾病(Parkinson’s disease)模型中黑质区域多巴胺能神经元的凋亡过程,而且发现在相同条件的药物诱导所建立的模型中,小鼠黑质区域AChE的表达量与多巴胺能神经元的损伤程度在一定程度上呈正相关关系。该研究为完善帕金森疾病发病过程中细胞凋亡调控网络提供新线索,也将有可能为帕金森疾病这种神经退行性疾病提供新靶标和候选性肽类新药物。
帕金森疾病作为常见的老年性神经退行性疾病,在60岁以上的老年人群中的发病率正逐年上升。其初期表现为四肢震颤,行为迟缓,肌肉僵直,晚期认知障碍和行为障碍将更为严重,甚至痴呆。帕金森最主要的病理改变是中脑黑质区域多巴胺能神经元的死亡,由此而引起纹状体内多巴胺含量显着性减少而致病。但是其确切病因还不清楚,被认为与遗传因素、环境因素、年龄老化、氧化应激相关。所以目前所使用的治疗手段只能改善症状,不能阻止病情的进展,也无法治愈疾病。
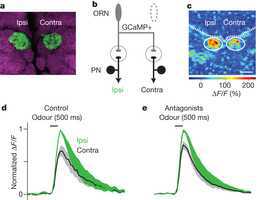
张学军研究组长期以来致力于研究AChE在细胞凋亡过程中发挥的作用。以往研究发现,几乎来源所有组织的凋亡细胞中,均能表达AChE。而且在肾脏缺血再灌注模型及糖尿病模型中,AChE也被证实参与到了细胞凋亡相关的病理过程中。猜测AChE可能在帕金森疾病发病过程中也起到一定的作用。期望通过建立帕金森疾病的细胞及动物模型研究AChE与帕金森疾病发病机理的关系。博士研究生张雪瑾等在张学军研究员的指导下,通过一系列的体外细胞实验和体内动物实验,发现无论是在体外1-methyl-4-phenylpyridinium(MPP+)细胞模型还是在体内1,2,3,6-tetrahydropyridine (MPTP)小鼠模型中,都证实了AChE参与了帕金森疾病模型中,中脑黑质区域多巴胺能神经元的凋亡过程。在进一步的研究中,利用AChE基因敲除小鼠建立帕金森疾病模型,发现AChE表达量较少的AChE基因敲除杂合子小鼠的的黑质区域多巴胺能神经元的细胞凋亡比例明显小于野生型小鼠,相应的细胞凋亡标志蛋白caspase系列蛋白剪切也明显减少。这一发现提示AChE表达的缺失对帕金森疾病模型中的多巴胺能神经元有一定的保护作用,为研究帕金森疾病的发病机理提供了新的思路。
该项工作得到了国家自然科学基金的支持。

DOI:10.1016/j.biocel.2012.11.015
PMC:
PMID:
Xuejin Zhang1, Lu Lu1, Shengjun Liu, Weiyuan Ye, Jun Wu, Xuejun Zhang,
The apoptosis pathway has been proposed to be involved in causing neuronal cell death in the pathogenesis of Parkinson's disease. However, the details of this pathway are poorly understood. Previous research has shown increased acetylcholinesterase expression during apoptosis in various cell types, which suggests that acetylcholinesterase has a potential role in neuronal cell death. In this study, we found that acetylcholinesterase protein expression increased and caspase-3 was activated in PC12 cells treated with 1-methyl-4-phenylpyridinium. Furthermore, the genetic or pharmacological inhibition of acetylcholinesterase was shown to protect PC12 cells from MPP+ induced apoptotic cell death. To study the function of acetylcholinesterase as a mechanism of neuronal cell death in vivo, we subsequently established a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine Parkinson's disease mouse model utilizing acetylcholinesterase-deficient mice. Studies in these mice revealed reduced dopaminergic neuron loss and lower expression levels of apoptotic proteins in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated heterozygous mice compared to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated wild-type mice. We conclude that it is highly probable that acetylcholinesterase is involved in the pathogenesis of the neurotoxin model of Parkinson's disease via apoptosis. Specifically, a deficiency or inhibition of acetylcholinesterase can decrease apoptosis and protect dopaminergic neurons in the neurotoxin model of Parkinson's disease.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JBC#
54
#乙酰胆碱#
61
#疾病模型#
105
#帕金森疾病#
80
#胆碱#
65
#多巴胺能神经元#
98