专家共识:前列腺穿刺
2016-07-08 中华医学会泌尿外科学分会中国前列腺癌联盟 《中华泌尿外科杂志》2016年4月第37
前列腺癌的流行病学特征有明显的地域和种族差异。在全球范围内,前列腺癌在男性恶性肿瘤中发病率占第2位,欧美国家前列腺癌的发病率高于亚洲国家。近年来,我国前列腺癌的发病率和病死率均呈现明显的持续增长趋势,1998年中国前列腺癌粗发病率为3.52/10万,至2008年发病率增加了212.5%,达到11.00/10万,10年间的年增长比例为12.1%;1998年中国男性前列腺癌死亡率为1.81/10万
前列腺癌的流行病学特征有明显的地域和种族差异。在全球范围内,前列腺癌在男性恶性肿瘤中发病率占第2位,欧美国家前列腺癌的发病率高于亚洲国家。近年来,我国前列腺癌的发病率和病死率均呈现明显的持续增长趋势,1998年中国前列腺癌粗发病率为3.52/10万,至2008年发病率增加了212.5%,达到11.00/10万,10年间的年增长比例为12.1%;1998年中国男性前列腺癌死亡率为1.81/10万,2008年增加了124.9%,达到4.07/10万,年增长率为8.4%。多数地区新确诊的患者中晚期比例高于欧美国家,这将对我国前列腺癌患者的治疗效果及长期生存产生直接影响。如何提高前列腺癌的早期诊断率是我国前列腺癌临床诊疗中面临的重要问题。目前,前列腺穿刺活检仍是确诊前列腺癌的金标准。临床上使用最为广泛的是超声引导下经直肠或经会阴前列腺系统穿刺活检,但此项技术在全国许多医院尚未普及,仍有医院通过手指引导下的穿刺来诊断前列腺癌。随着影像学技术的进步,多参数MRI诊断前列腺癌的敏感性和特异性越来越高,基于多参数、超声造影、超声弹性成像的靶向穿刺、融合穿刺技术的快速进展,有效提高了穿刺阳性率,但新技术对硬件和操作技巧的要求更高,推广普及难度较大。此外,关于前列腺穿刺活检的指征、穿刺人路、穿刺针数、重复穿刺指征以及穿刺相关并发症的预防和处理方面,国内尚无统一的规范。
为普及穿刺活检知识、规范临床操作,提高我国前列腺癌早期诊断整体水平,中华医学会泌尿外科学分会和中国前列腺癌联盟专家组结合各国指南及此领域热点问题、相关文献,编制此共识。
一、前列腺初次穿刺指征和禁忌证
中国前列腺癌联盟(CPCC)开展的一项前列腺穿刺活检现状调查结果显示,我国前列腺穿刺活检患者与欧美国家相比具有PSA高、前列腺体积小、Gleason评分高、阳性率低等特点。本共识建议的前列腺穿刺指征包括:①直肠指检(digital rectal examination,DRE)发现前列腺可疑结节,任何PSA值;②经直肠前列腺超声(transrectaluhrasonography,TRUS)或MRI发现可疑病灶,任何PSA值;③PSA>10μg/L;@PSA 4~10μg/L,f/t PSA可疑或PSAD值可疑。
前列腺穿刺的禁忌证包括:①处于急性感染期、发热期;②有高血压危象;③处于心脏功能不全失代偿期;④有严重出血倾向的疾病;⑤处于糖尿病血糖不稳定期;⑥有严重的内、外痔,肛周或直肠病变。
二、前列腺穿刺活检术的实施
1.穿刺术前常规检查:患者行前列腺穿刺活检术前应常规行血、尿、粪三大常规及凝血功能检查,有肝肾功能异常病史者需复查肝。肾功能。因前列腺穿刺活检术会引起前列腺局部MRI影像的改变,故如需通过MRI评估临床分期,通常建议在前列腺穿刺活检前进行。基于多参数MRI的靶向穿刺在初次穿刺中并不能显著提高穿刺阳性率,在多中心前瞻性临床研究得出进一步结论前,不推荐多参数MRI作为初次穿刺之前的常规检查。
2.预防性抗生素的应用:经直肠超声引导下前列腺穿刺活检术之前,应常规口服或静脉预防性应用抗生素,喹诺酮类抗生素是首选,目前的临床数据显示单次应用与用药1~3d的效果相当。穿刺术后的严重感染多与喹诺酮类药物耐药有关。经会阴前列腺穿刺前不需要预防性应用抗生素。
3.肠道准备:经直肠前列腺穿刺活检前清洁肠道是常规操作,开塞露可代替灌肠,建议穿刺前碘伏清洁肠道。
4.围手术期抗凝及抗血小板药物的使用:对于有心脑血管病风险、支架植入病史的长期口服抗凝或抗血小板药物的患者,围手术期应综合评估出血风险及心脑血管疾病风险,慎重决定相关药物的使用。尽管有前瞻性研究结果表明,前列腺穿刺时不停用小剂量阿司匹林并不增加严重出血的风险,但多数学者仍建议围手术期停用抗凝及抗血小板药物。阿司匹林及其他非甾体类抗炎药穿刺前应停用3-5d,氯吡格雷应停用7d,噻氯匹定应停用14d,双香豆素建议停用4~5d。
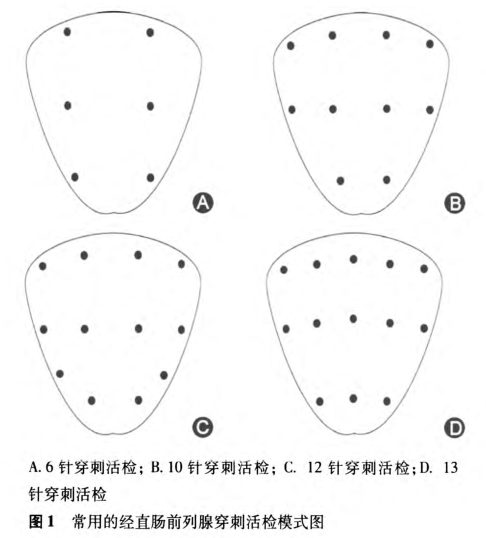
5.穿刺针数和部位:Hodges等引于1989年提出前列腺6针系统穿刺法,但穿刺阳性率仅为20%~30%,已不作为初次穿刺的首选。建议前列腺体积为30-40 ml的患者,需接受不少于8针的穿刺活检,推荐10—12针系统穿刺作为基线(初次)前列腺穿刺策略。穿刺针数的增加不显著增加并发症的发生率。饱和穿刺可作为一种穿刺策略。
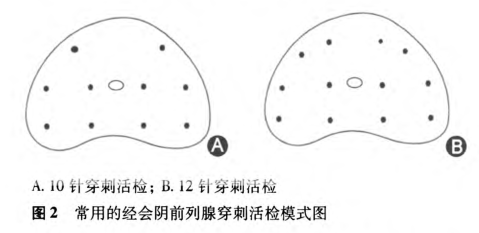
常用的经直肠。和经会阴前列腺穿刺活检模式图见图1和图2。
6.麻醉:经直肠和经会阴前列腺穿刺对麻醉的要求不同。通常大多数患者在经直肠穿刺中未经麻醉也能很好耐受。超声引导下前列腺周围阻滞是经直肠前列腺穿刺麻醉的最优选择,其效果优于经直肠灌注局麻药物。如果是经会阴前列腺穿刺,则需要增加对进针区域皮肤的局部麻醉。
7.穿刺信息的记录:穿刺过程中应详细记录穿刺相关信息,包括前列腺各径线长度、超声异常信号的大小及位置、穿刺标本序号对应的大概位置。
三、前列腺穿刺相关并发症及处理
穿刺后主要并发症包括感染、血精、血尿、血便、发热、尿潴留、迷走神经反射、前列腺炎、附睾炎等。
1.血尿:血尿是经直肠前列腺穿刺的常见并发症,主要是由于穿刺针刺破尿道或膀胱引起。穿刺术前停用抗凝血类药物,穿刺时避开尿道和膀胱减少穿刺损伤,能够有效减少血尿的发生。严重血尿时可留置三腔导尿管牵引压迫止血。
2.血便:穿刺针损伤直肠黏膜可引起血便,血便的发生率较低,常在穿刺术后很快消失。如术中出现直肠出血,可利用手指压迫出血点进行止血。
3.感染:前列腺穿刺术后感染的发生率为0.1%-7.0%,严重感染可导致患者死亡。严重感染多与喹诺酮类药物耐药有关,如感染无法控制,应及时行细菌培养并调整抗菌药物使用策略。
4.迷走神经反射:前列腺穿刺引起的患者过度紧张和不适可导致中度或严重的血管迷走神经反射,发生率为1.4%~5.3%;主要表现为呕吐、心动过缓和血压下降。当出现血管迷走神经反射时,可将患者体位调整为头低脚高位并静脉补液,以缓解相关症状。
四、穿刺结果预测及规范化的病理报告
患者年龄、PSA、前列腺体积、异常DRE、前列腺癌抗原3(prostate eaneer antigen 3,PCA3)、前列腺健康指数(prostatehealth index,PHI)心引等被认为是前列腺穿刺阳性的预测因素;多种量表被用于预测前列腺穿刺结果,但尚无得到多中心验证的适合中国人的量表。
前列腺穿刺病理报告应包括单针病理、Gleason评分及肿瘤百分比,以及穿刺样本总Gleason评分。
五、重复穿刺
当第1次前列腺穿刺结果为阴性,但DRE、复查PSA或其他衍生物水平提示可疑前列腺癌时,可考虑再次行前列腺穿刺。如具有以下情况需要重复穿刺:①首次穿刺病理发现非典型性增生或高级别PIN,尤其是多针病理结果如上;②复查PSA>10μ/L;③复查PSA 4~10μg/L,%fPSA、PSAD值、DRE或影像学表现异常,如TRUS或MRI检查提示可疑癌灶,可在影像融合技术下行兴趣点的靶向穿刺;@PSA 4~10μg/L,%fPSA、PSAD值、DRE、影像学表现均正常的情况下,每3个月复查PSA。如PSA连续2次>10μg/L,或PSA速率(PSAV)>0.75μg/(L·年),需要重复穿刺。
重复穿刺前除常规检查外,推荐行多参数MRI检查,基于多参数MRI的靶向穿刺可显著提高重复穿刺阳性率并避免漏诊高危前列腺癌。关于重复穿刺的时机,两次穿刺间隔时间尚有争议,建议3个月或更长,待组织结构完全恢复。
重复穿刺前如影像学发现可疑灶,应对可疑灶行靶向穿刺。
六、前列腺系统穿刺的局限性及新策略
经直肠或经会阴前列腺系统穿刺活检术的主要局限在于假阴性、漏诊高危前列腺癌和过度诊断。如何在提高穿刺阳性率的同时避免过度诊断是前列腺癌早期诊断中面临的巨大挑战。近年来,以超声增强造影、超声弹性成像和多参数MRI为靶向的前列腺穿刺活检术在发现有临床意义前列腺癌、避免过度诊断方面展现了明显的优势。
MRI引导的靶向穿刺可在MRI引导下直接对可疑灶进行取材,其精确性最高。已有多项研究显示,MRI引导前列腺穿刺活检可以提高重复穿刺时高级别前列腺癌的检出率。但操作相对复杂,且价格昂贵,有一定推广难度。
MRI/TRUS融合技术结合了MRI定位的精度与经直肠超声引导穿刺的便利,在显著提高穿刺阳性率的同时,能够增加发现有临床意义的前列腺癌的比例并避免发现无临床意义的前列腺癌,与MRI下的穿刺相比操作更加便利。
附录
1.前列腺穿刺推荐操作设备:①B超机;②经直肠超声探头(双平面);③活检穿刺枪和穿刺针;④穿刺定位架。
2.经直肠前列腺系统穿刺推荐操作步骤:①患者取左侧卧位,臀部朝向术者,常规消毒铺巾。②将肛门镜插入肛门、拔下内芯,以碘伏棉球消毒直肠壁。③取出肛门镜,注人利多卡因胶浆对进针部位肠壁黏膜做局部麻醉。④在直肠超声探头的晶体面涂以耦合剂,套上无菌乳胶套,将探头缓缓插入直肠进行探查,深度6~10 cm,使声束指向前列腺方向。⑤根据前列腺超声图像,记录前列腺各径线长度,计算前列腺体积。观察前列腺异常回声信号,并记录异常回声位置、大小。⑥调整探头位置改变穿刺引导线指向,在前列腺左侧叶的尖部、中部和基底部各穿刺1针;调整探头位置在左侧叶外周带外侧穿刺2~3针。同法对右侧叶进行穿刺。穿刺总针数为10—12针。⑦从穿刺枪上取下活检标本,对标本末端进行染色,以区分标本头端和尾端,然后将标本放人含4%甲醛标本瓶中。⑧穿刺完毕后取出探头,插入肛门镜,以碘伏棉球消毒直肠。观察直肠壁,如有明确出血点,首选压迫止血。待直肠壁无明确出血后,塞入无菌干燥纱布,4~6h后取出,观察纱布表面有无明显血染。
3.经会阴穿刺:①患者取截石位,常规消毒铺巾,向上牵拉阴囊暴露会阴部,肛门上方2 cm、中线旁开1.5 cm处为穿刺点。②注射针抽取2%利多卡因,经直肠超声引导下,进针至前列腺包膜,对包膜及尖部进行阻滞麻醉。注意避开血管富集区,边退针边推人2%利多卡因,推注前先回抽确认针尖不在血管内。③将装有穿刺模板的直肠超声探头缓缓插入直肠进行检查(具体步骤同上)。④在直肠超声定位下通过穿刺模板进行前列腺穿刺,对前列腺左、右侧叶基底部以及体部至尖部各穿1针;调整探头位置,对左、右侧外周带各穿2针,穿刺总针数为10针。⑤从穿刺枪上取下活检标本,对标本末端进行染色,以区分标本头端和尾端,然后将标本放入标本瓶中。⑥穿刺完毕后消毒加压包扎会阴部进针点。
执笔专家:高旭
参与讨论和审定专家(按单位汉语拼音排序):安徽医科大学第一附属医院泌尿外科(梁朝朝),北京大学第一医院泌尿外科(周利群),北京医院泌尿外科(王建业),第二军医大学长海医院泌尿外科(高旭、孙颖浩、许传亮),复旦大学附属肿瘤医院泌尿外科(叶定伟,朱耀),华中科技大学同济医学院附属同济医院泌尿外科(王少刚,叶章群),上海交通大学医学院附属仁济医院泌尿外科(黄翼然),四川大学华西医院泌尿外科(王坤杰,魏强),天津医科大学第二医院泌尿外科(徐勇),西安交通大学附属第一医院泌尿外科(贺大林),浙江大学医学院附属第一医院泌尿外科(谢立平),中国医科大学附属第一医院泌尿外科(毕建斌,孔垂泽),中国医学科学院北京协和医院泌尿外科(李汉忠),中山大学附属第三医院泌尿外科(高新),中山大学孙逸仙纪念医院泌尿外科(黄健,林天歆)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好文章,学习了,谢谢
86
文章不错
91
马上照着做。
81
值得学习
79
讲的很详细
99
#专家共识#
0
其实有很多方面要注意
81
#穿刺#
66
总结的很全面
75