JCEM:补充维生素D可改善不育男性的糖/脂代谢稳态
2021-09-14 Nebula MedSci原创
大剂量维生素 D 补充剂对不育男性的葡萄糖稳态和高密度脂蛋白胆固醇水平有益
多项研究表明,维生素 D 缺陷与葡萄糖和脂质代谢受损(包括糖尿病)相关。维生素 D 缺乏的症状有骨痛、超重/肥胖、心情烦闷等。性腺功能受损的男性患代谢综合征和死亡的风险更高,而维生素 D 状态可能是一种可逆的调节剂。
这是一项单中心、双盲、随机、安慰剂为对照的临床试验,旨在评估连续每天补充维生素 D 和钙 150 天对不育男性的葡萄糖和脂质稳态的影响。
共招募了 307 位不育男性随机(1:1)被随机分成两组,实验组(n=151)受试者接受单剂量 30 万单位的胆钙化醇后,每日服用 1400 单位胆钙化醇和 500 mg 钙;安慰剂组(n=156)接受相同模式的安慰剂,持续干预 150 天。评估的代谢参数包括空腹血糖、HbA1c、空腹血清胰岛素、胰岛素抵抗的稳态模型评估 (HOMA-IR)、空腹血浆胆固醇和甘油三酯。
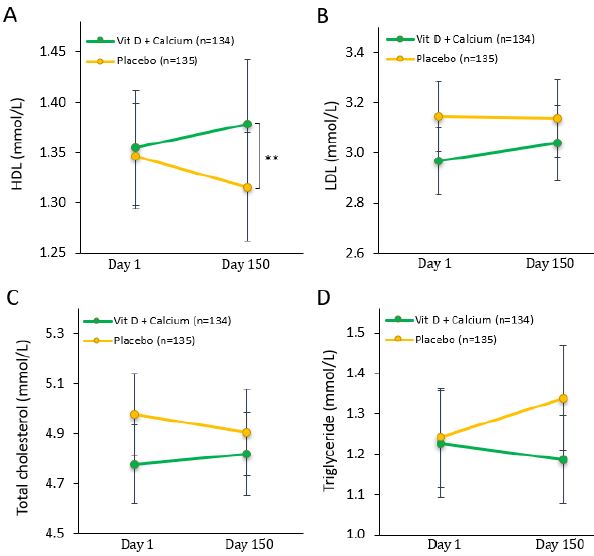
两治疗组多项脂代谢参数的变化
补充维生素 D 的男性的维生素 D 状态获得了改善,而安慰剂组男性的维生素 D 状态发生了恶化,其特征是血清甲状旁腺激素 (PTH) 升高。在试验结束时,与安慰剂治疗组相比,服用维生素 D 补充剂的男性的空腹血清胰岛素浓度降低了 13%(65 vs 74 pmol/L,p=0.018),HOMA-IR 降低了 19%(2.2 vs 2.7,p=0.025)。此外,实验组男性的高密度脂蛋白(HDL)胆固醇水平明显低于安慰剂组(1.32 vs 1.38,p=0.008)。
综上所述,大剂量维生素 D 补充剂对不育男性的葡萄糖稳态和高密度脂蛋白胆固醇水平有益。
原始出处:
Holt Rune,Pedersen J?rgen Holm,Dinsdale Elsa et al. Vitamin D supplementation improves fasting insulin levels and HDL cholesterol in infertile men.[J] .J Clin Endocrinol Metab, 2021,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
106
#稳态#
111
#JCEM#
126
#脂代谢#
112
?!:。。low,
120