JCRS:白内障术后疗效满意度相关因素调查
2014-07-18 佚名 dxy
白内障手术旨在改善患者视力、提高患者生活质量,但仅仅将视力检测作为唯一评估手术效果的指标是远远不够的,更重要的是患者自觉的视功能改善及手术效果、满意度。如何做漂亮手术,提高患者主观满意度是每位术者的终极目标。 对瑞典41家白内障中心术后患者的断面研究显示:无并发眼病、年轻、女性、等候手术时间短、术前视力差、术后视力好的白内障患者自觉视功能改善更明显;术前无并发眼病、术后矫正远视力(CDVA)好的
白内障手术旨在改善患者视力、提高患者生活质量,但仅仅将视力检测作为唯一评估手术效果的指标是远远不够的,更重要的是患者自觉的视功能改善及手术效果、满意度。如何做漂亮手术,提高患者主观满意度是每位术者的终极目标。
对瑞典41家白内障中心术后患者的断面研究显示:无并发眼病、年轻、女性、等候手术时间短、术前视力差、术后视力好的白内障患者自觉视功能改善更明显;术前无并发眼病、术后矫正远视力(CDVA)好的患者整体满意度也较高,相应结果发表于2014年J Cataract Refract Surg。
Magnus Grimfors等对2008年至2011年期间每年3月份瑞典国家白内障中心登记的共10979名患者进行Catquest-9SF问卷调查,观察患者自我感知的术后3月时视功能的改善情况、客观的术后视功能情况及患者整体满意度,最终入选10364名患者,所有问卷结果均经Rash分析将非参数分级结果转换为参数化数据后进行统计分析。
问卷中2个问题与整体日常生活完成有关,7个与具体的日常生活行为相关相关(阅读报纸、辨识熟人、价签识别、崎岖地面的行走力、字幕辨识、满足手工木工等作业的要求、既往爱好的完成能力),相应选项为:非常困难、比较困难、稍有困难、没有困难及无法判定。
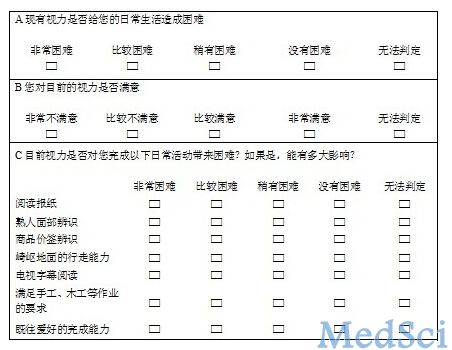
图 Catquest-9SF问卷内容
此研究结果有利于医生为患者选择手术时机、预测手术预后,有助于更好的因人而异地与患者沟通手术相关事宜。
原始出处
Grimfors M1, Mollazadegan K2, Lundström M1, Kugelberg M1.Ocular comorbidity and self-assessed visual function after cataract surgery.J Cataract Refract Surg. 2014 Jul
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









问卷挺简单的
178
#相关因素#
64
#满意度#
68
#JCR#
68
#CRS#
98