ASCO 2018:同步放化疗联合pembrolizumab巩固治疗用于不可切除III期NSCLC的II期研究
2018-06-01 MedSci MedSci原创
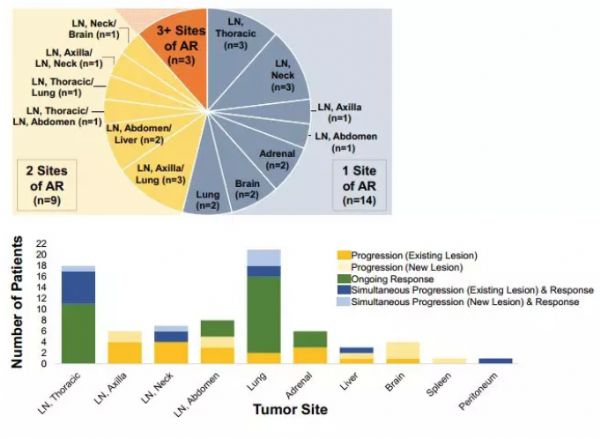
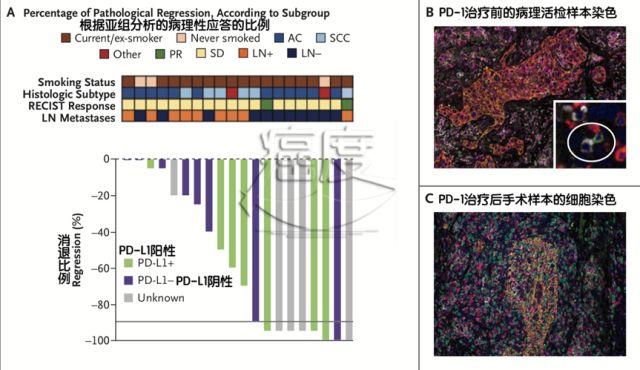
同步放化疗联合pembrolizumab巩固治疗用于不可切除III期NSCLC的II期研究:Hoosier癌症研究网络LUN 14-179试验摘要编号:8500 时间:6月4日8:00 AM~11:00 AM 专场:肺癌 形式:口头报告 背景:同步放化疗(CRT)是不可切除III期NSCLC的标准治疗方案。最近PACIFIC III 期临床研究显示,与安慰剂
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
0
#III#
54
#PE#
49
#Pembro#
54
#mAb#
0
#Pembrolizumab#
48
#放化疗#
49
#同步放化疗#
62
#III期#
66