Lancet子刊:南方医科大学李国新等合作团队开发了一种深度学习模型,可实时、准确预测腹膜复发风险和无病生存期
2022-09-12 iNature iNature
深度学习模型可以准确预测胃癌患者的腹膜复发和生存情况。 需要前瞻性研究来检验该模型在结合临床病理学标准指导个性化治疗方面的临床效用。
腹膜复发是胃癌根治性手术后的主要复发形式,且预后不佳。准确的个体化腹膜复发预测对于确定哪些患者可能从强化治疗中受益至关重要。该研究旨在建立胃癌腹膜复发和预后的预测模型。
2022年5月,斯坦福大学李瑞江、南方医科大学李国新及中山大学周志伟共同通讯(南方医科大学江玉明为第一作者)在Lancet Digital Health(IF=37)在线发表题为“Predicting peritoneal recurrence and disease-free survival from CT images in gastric cancer with multitask deep learning: a retrospective study” 的研究论文,在这项包含2320名患者的回顾性多机构研究中,开发了一种多任务深度学习模型,利用术前CT图像同时预测腹膜复发和无病生存。训练队列(n=510)和内部验证队列(n=767)的患者来自南方医科大学。外部验证队列的患者(n=1043)来自中山大学癌症中心。该研究评估了该模型的预后准确性及其与化疗反应的关系。此外,该研究评估了该模型是否能提高临床医生预测腹膜复发的能力。
深度学习模型在预测腹膜复发方面具有始终如一的高精度。当被人工智能(AI)模型告知时,肿瘤医生预测腹膜复发的敏感性和评分者之间的一致性得到了提高。在多变量分析中,该模型独立于临床病理学变量预测腹膜复发和无病生存。对于预计腹膜复发风险高且生存期低的患者,辅助化疗与两种 II 期疾病和 III 期疾病的无病生存期改善相关。相比之下,对于预计腹膜复发风险低且生存率高的患者,化疗对无病生存率没有影响。对于其余患者,化疗的益处取决于分期:只有 III 期疾病患者才能从化疗中获益。总之,深度学习模型可以准确预测胃癌患者的腹膜复发和生存情况。 需要前瞻性研究来检验该模型在结合临床病理学标准指导个性化治疗方面的临床效用。

胃癌是世界范围内最常见的恶性肿瘤之一,也是导致癌症死亡的主要原因尽管多方式治疗取得了进展,但复发率仍然很高。腹膜是手术治疗后最常见的复发部位。由于全身化疗在腹膜疾病中只有适度的生存优势,新的治疗方法正在积极研究中。几次腹腔内加热化疗的试验已显示出控制疾病的良好效果。然而,由于该手术与术后并发症(包括消化道瘘、粘连性肠梗阻和全身脓毒症)的发生率增加有关,因此其长期生存益处尚不清楚。因此,准确的个体化预测高危人群腹膜复发将是至关重要的,以选择患者最有可能受益于新的治疗,如腹腔内加热化疗。
深度学习是一种从医学图像中提取信息的强大方法,已显示出对预后预测的希望,包括胃癌。传统上,深度学习模型被设计用于执行单一任务,(例如,预测一个特定的终点,如总生存期)。相比之下,在多任务学习中,多个任务是通过单一模型同时学习的,多任务学习的数据效率更高,并已被证明在许多应用中减少过拟合和提高模型的泛化能力,包括计算机视觉,药物发现和疾病诊断。研究者开发了一种多任务深度学习模型,利用术前CT图像同时预测腹膜复发和无病生存。研究者还将腹膜复发和无病生存期的信息整合到这个模型中,以确定哪些患者可以从辅助化疗中获益。
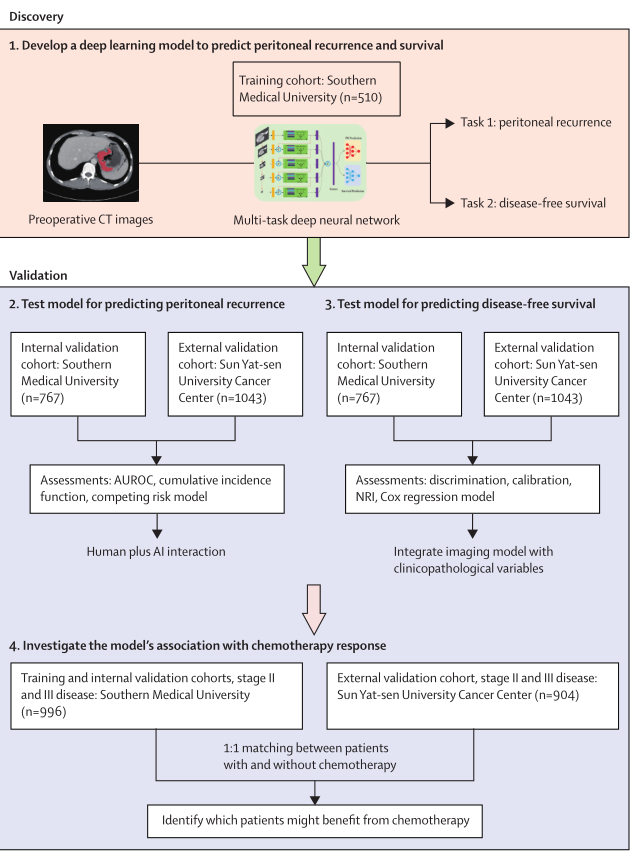
研究设计用于开发和验证预测腹膜复发和无病生存的深度学习模型(图源自Lancet Digital Health )
在这项包含2320名患者的回顾性多机构研究中,开发了一种多任务深度学习模型,利用术前CT图像同时预测腹膜复发和无病生存。训练队列(n=510)和内部验证队列(n=767)的患者来自南方医科大学。外部验证队列的患者(n=1043)来自中山大学癌症中心。该研究评估了该模型的预后准确性及其与化疗反应的关系。此外,该研究评估了该模型是否能提高临床医生预测腹膜复发的能力。
深度学习模型在预测腹膜复发方面具有始终如一的高精度:在训练队列(受试者工作特征曲线下面积 [AUC] 0·857;95% CI 0·826–0·889)、内部验证队列(0·856;0·829–0·882)和外部验证队列(0·843;0·819–0·866)。当被人工智能(AI)模型告知时,肿瘤医生预测腹膜复发的敏感性和评分者之间的一致性得到了提高。该模型能够预测无病生存:训练队列(C-index 0·654;95% CI 0·616–0·691)、内部验证队列(0·668;0·643–0·693)和外部验证队列(0·610; 0·583–0·636)。在多变量分析中,该模型独立于临床病理学变量预测腹膜复发和无病生存(所有p<0·0001)。
对于预计腹膜复发风险高且生存期低的患者,辅助化疗与两种 II 期疾病(风险比 [HR] 0·543 [95% CI 0·362–0·815] ; p=0·003) 和 III 期疾病 (0·531 [0·432–0·652]; p<0·0001)的无病生存期改善相关。相比之下,对于预计腹膜复发风险低且生存率高的患者,化疗对无病生存率没有影响。对于其余患者,化疗的益处取决于分期:只有 III 期疾病患者才能从化疗中获益(HR 0·637 [95% CI 0·484–0·838];p=0·001)。
总之,深度学习模型可以准确预测胃癌患者的腹膜复发和生存情况。 需要前瞻性研究来检验该模型在结合临床病理学标准指导个性化治疗方面的临床效用。
参考消息:
https://www.thelancet.com/digital-health
1211894+70000+1549+97816。+130000
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#医科大学#
0
#Lancet#
137
#复发风险#
109
谢谢分享
89
#深度学习模型#
82
#生存期#
102
#腹膜#
127