Nat Commun:改善伤口愈合的新靶点
2017-05-21 sunshine2015 来宝网
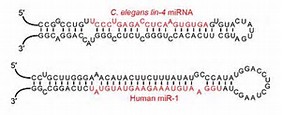
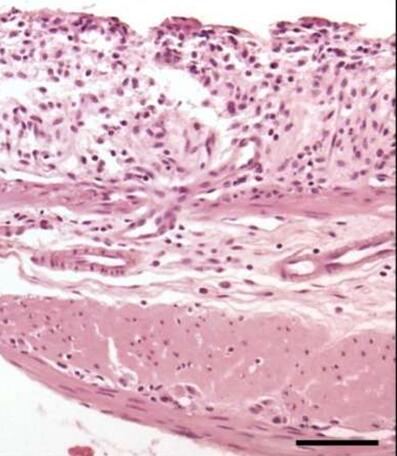
MicroRNA是新的治疗剂的有趣靶标结构。它们可以通过合成抗氧化剂阻断。然而,到目前为止,仅在局部使用这些数据是不可能的。歌德大学法兰克福的研究人员现在已经成功地实现了这一点,在光诱导型抗生素的帮助下治疗伤口愈合受损。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
116
#COMMUN#
66
#新靶点#
68
#伤口愈合#
0
学习了。
115