JACC:PRKAG2综合征的临床特征和自然病程研究
2020-07-13 MedSci原创 MedSci原创
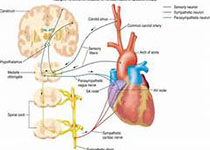
PRKAG2基因变异可导致一种以心肌病、传导疾病和心室预激为特征的综合征,到目前为止,只有少数病例报告,对该病的自然史了解甚少。本研究的目的是在一个大型多中心欧洲队列中描述PRKAG2变异的表型和自然
PRKAG2基因变异可导致一种以心肌病、传导疾病和心室预激为特征的综合征,到目前为止,只有少数病例报告,对该病的自然史了解甚少。本研究的目的是在一个大型多中心欧洲队列中描述PRKAG2变异的表型和自然病程。
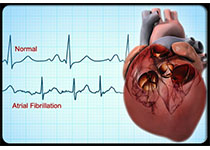
本研究纳入分析了来自27个多中心的90例PRKAG2基因变异的患者(男性占53%,平均年龄33岁)。在首次评估中,93%的患者的心功能评级为纽约心功能I或II级,最大左室壁厚18±8mm,左室射血分数61±12%。有60名患者在基线水平时存在左室壁肥厚。30例患者(33%)有心室预激或接受过旁路消融;17例(19%)有起搏器植入,16例(18%)有心房颤动。经过平均6年时间的随访,71%患者有左室肥厚,29%有房颤,21%患者需要植入新的起搏器,14%需要心衰住院治疗,8%出现心源性死亡,4%需要心脏移植,13%患者死亡。
研究结果显示,PRKAG2综合征是一种进行性心肌病,其特征是房颤、传导疾病、晚期心力衰竭和危及生命的心律失常。预激和严重左室肥厚的典型特征并不一致,在年轻时发生房颤或需要永久起搏器的左室肥厚患者应考虑诊断。
原始出处:
Angela L et al.Clinical Features and Natural History of PRKAG2 Variant Cardiac Glycogenosis.JACC.2020 July.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
60
#临床特征#
64
#自然病程#
68
#ACC#
65
#综合征#
58