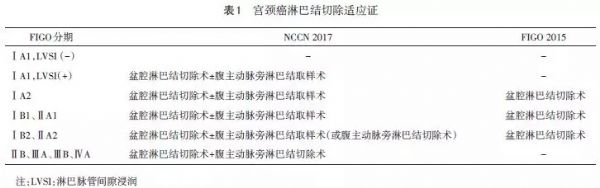
宫颈癌淋巴结切除适应证和争议
2018-01-05 王伟、姚书忠 中国实用妇科与产科杂志
淋巴结切除是评估淋巴结转移状态的主要手段,本文就宫颈癌淋巴结切除适应证和相关争议做一介绍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#适应证#
61
不错的文章.值得拥有
71
深度好文.谢谢分享
81
#淋巴结#
53
#宫颈#
62
非常好的文章.学习了
79