Ann Thorac Surg:上海胸科医院韩宝惠等发现EBUS-TBNA对可疑胸内结核有很高诊断价值
2013-11-11 sd3212 DXY 发表于威斯康星
支气管内超声引导下经支气管针吸活检(EBUS-TBNA)是一种微创操作,其对纵隔及肺门淋巴结的诊断评估具有很高的敏感性,但它在诊断胸内结核病(TB)方面的作用尚未明确。为此,来自上海交通大学附属上海市胸科医院内镜中心和肺内科的韩宝惠及其同事进行了一项研究,研究结果发表于2013年9月12日出版的《胸外科年鉴》(Ann Thorac Surg)杂志上。研究结果显示:EBUS-TBNA对于可疑的胸内结
支气管内超声引导下经支气管针吸活检(EBUS-TBNA)是一种微创操作,其对纵隔及肺门淋巴结的诊断评估具有很高的敏感性,但它在诊断胸内结核病(TB)方面的作用尚未明确。为此,来自上海交通大学附属上海市胸科医院内镜中心和肺内科的韩宝惠及其同事进行了一项研究,研究结果发表于2013年9月12日出版的《胸外科年鉴》(Ann Thorac Surg)杂志上。研究结果显示:EBUS-TBNA对于可疑的胸内结核具有很高的诊断价值。通过对胸内淋巴结及与气管支气管壁相邻处肺部病变的针吸穿刺检查,可以提高对此类病变的诊断率。【原文下载】
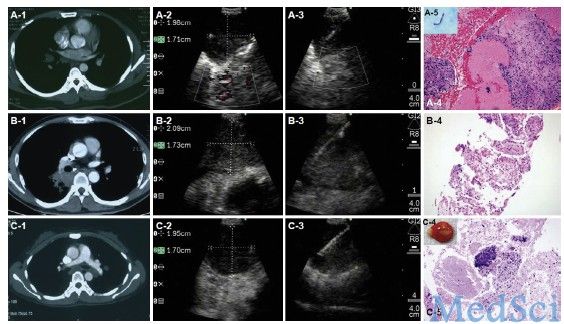
该研究是一项前瞻性临床研究,其研究对象主要为从2010年12月到2011年12月期间在某胸科临床医学中心就诊的59例疑似肺结核患者。这些患者均伴有适合于行EBUS-TBNA检查的胸部淋巴结病变或肺内病变。研究者记录并分析了受试者的支气管镜检查结果、EBUS-TBNA检查过程和活检病理结果、微生物检验结果等内容。
研究主要结果为:在59例符合条件的受试者中,41例确诊为肺结核,5例肺癌、7例炎症、6例结节病。其中通过EBUS-TBNA检查诊断结核病的敏感性为85%,特异性为100%;其阳性预测值和阴性预测值则分别为100%和75%,准确度为90%。在41例确诊为肺结核的受试者中,病理结果符合结核病表现者占80%(33/41例),痰涂片阳性者占27%(11/41例)。在41例确诊肺结核的患者中,共37例进行了结核菌培养,其中46%(17例)培养为阳性。此外,研究者对上述41例肺结核患者的80个纵隔及肺门淋巴结及5处肺内病变进行了活组织检查。
多因素Logistic回归分析显示,受累淋巴结或病变的短轴直径是病理、结核菌涂片或结核菌培养阳性的独立危险因素。而病理显示组织坏死则是一个与结核菌培养阳性相关的独立危险因素。
该研究结果表明:支气管内超声引导下经支气管针吸活检对于可疑的胸内结核具有很高的诊断价值。通过对胸内淋巴结,以及与气管支气管壁相邻处肺部病变进行针吸穿刺检查,可以提高对此类病变的诊断率。
原文出处:
Sun J, Teng J, Yang H, Li Z, Zhang J, Zhao H, Garfield DH, Han B.Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in Diagnosing Intrathoracic Tuberculosis.Ann Thorac Surg. 2013 Sep 12. pii: S0003-4975(13)01540-3. doi: 10.1016/j.athoracsur.2013.07.005.【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EBUS-TBNA#
63
#诊断价值#
64
#韩宝惠#
58
#THORAC#
62
#结核#
74