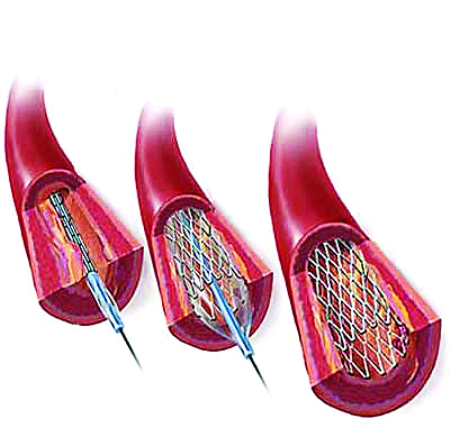
中国更新STEMI指南:建立区域救治网络,不建议急诊干预非梗死动脉
2015-06-09 中国循环杂志 中国循环杂志
近期中华医学会心血管病学分会更新了《急性ST段抬高型心肌梗死诊断和治疗指南》,上一版指南是2010年公布的。新一版指南在理念上有了进一步提高,结合了我国近期工作和过去一段时间的研究成果,做出了适合目前国情的推荐。比如,指南指出,建立区域协同救治网络和规范化胸痛中心,通过远程无线系统提前将心电图传输到相关医院,对确诊急性STEMI患者进行现场分诊,优先可行直接经皮冠状动脉介入治疗(PCI)的医院,可
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











有内容很值得学习
158
#不建议#
70
有用
130
#STEM#
73
culprit trial的结果好像支持干预?
166
看看
165