Cell子刊:为何肺炎更偏爱人类?
2016-09-04 佚名 生物谷
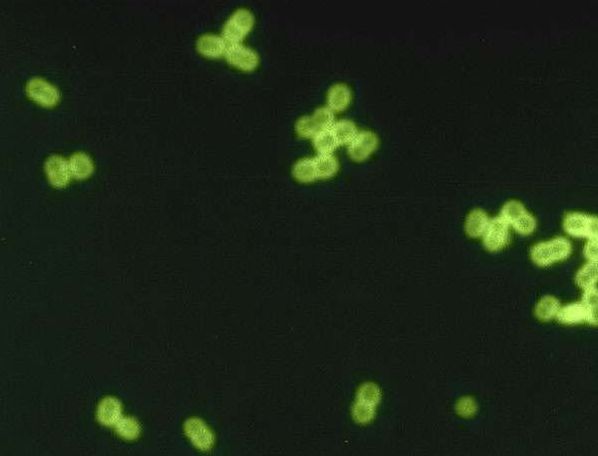
图片来源:www.phys.org 近日,刊登在国际杂志Cell Host & Microbe上的一项研究报告中,来自卡罗琳学院的研究人员通过研究表示,人类鼻腔中糖分子的特殊突变或可帮助解释为何人类相比其它动物更容易患上肺炎球菌感染,该研究或将帮助研究者开发抵御多种类型肺炎球菌感染的广谱性疫苗。 肺炎链球菌自然状态下存在于儿童和成年人的鼻腔中,但同时其又是常见感染性疾病的发病根本原因,
图片来源:www.phys.org
近日,刊登在国际杂志Cell Host & Microbe上的一项研究报告中,来自卡罗琳学院的研究人员通过研究表示,人类鼻腔中糖分子的特殊突变或可帮助解释为何人类相比其它动物更容易患上肺炎球菌感染,该研究或将帮助研究者开发抵御多种类型肺炎球菌感染的广谱性疫苗。
肺炎链球菌自然状态下存在于儿童和成年人的鼻腔中,但同时其又是常见感染性疾病的发病根本原因,肺炎链球菌常常会引发严重的脑膜炎和肺炎,相比其它动物而言,其会引发较为严重的感染,但具体原因目前科学家们并不清楚。
鼻腔粘液中包含了一种特殊的糖分子-唾液酸,肺炎链球菌会利用唾液酸作为能量来进行生长和存活,在特殊酶类的帮助下细菌会释放唾液酸会被转化成为细菌生长繁殖的能量;本文研究中,研究者发现,人类机体中存在的唾液酸能够使得肺炎链球菌更好地进行生长,同时相比在其它哺乳动物中发现的突变体而言,唾液酸还能够使得肺炎链球菌对机体的免疫防御产生较强的耐受性。
研究者对小鼠进行工程化操作,使其发生突变产生和人类机体一样形式的唾液酸,随后他们发现,相比对照组而言,这些被研究的小鼠更容易发生严重的肺炎球菌感染;研究者Birgitta Henriques-Normark教授说道,我们发现,人类机体的特殊糖分子突变体能够促进细菌产生大量酶类从而释放肺炎链球菌所需要的能量来源,而这无疑会增加人类鼻粘膜中肺炎链球菌的生长繁殖,此外细菌摄入较多的唾液酸也会诱发名为htrA蛋白的产生,该蛋白可以抵御一定的氧化性应激压力,而机体免疫系统常常会利用氧化性压力来抵御感染。
本文研究清晰地揭示了肺炎链球菌引发人类严重感染的机制和方式,相关研究数据或可帮助研究人员开发出更加高效的疫苗来抵御人类感染多种致病性的肺炎链球菌,同时也能够帮助改善当前的疫苗开发体系。
原始出处
Karina Hentrich, Jonas Löfling, Anuj Pathak, Victor Nizet, Ajit Varki, Birgitta Henriques-Normark.Streptococcus pneumoniae Senses a Human-like Sialic Acid Profile via the Response Regulator CiaR.Cell Host & Microbe.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
41
#CEL#
55
很好,不错,以后会多学习
65
讲的很好
84
谢谢,学习了。
78