患者女性,18岁,因出现上腹不适和反复性腹胀腹泻而来院就诊。

随即,该女患者又接受了胃镜检查,在十二指肠可见大量的结节样病变(如图A)。取活体组织检查发现,正常的绒毛固有层中淋巴滤泡与结节性淋巴样增生病变一致(如图B)。
做进一步检查评估发现,该患者患有低球蛋白血症和IgG、IgA以及IgM血清水平偏低。
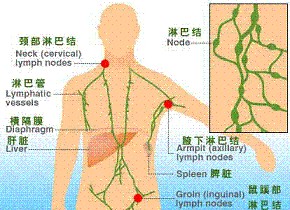
根据该患者的临床症状以及检查结果,会诊医师诊断其患上了结节性淋巴组织增生性免疫缺陷病。
在临床上,患有常见变异型免疫缺陷的患者中约有20%发生结节性淋巴组织增生容易被误诊为胃肠道息肉。
结节性淋巴组织增生的发病有可能与患者经常腹泻和营养吸收不良有关,相反,其他那些没有发生腹泻和营养吸收不良症状的患者反而不容易发病。
最后,该患者接受了甲硝唑药物治疗。另外,医生告知其由于患有免疫缺陷病,因此存在很大的感染风险。
原始出处:
Vishal Sharma, M.D., D.M.Arvind Ahuja, M.D. Nodular Lymphoid Hyperplasia.N Engl J Med 2016.July 21, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









文章很好,继续关注
91
不错哦,会学到很多
100
很好,不错,以后会多学习
94
#结节性#
56