JACC:多摄入海产品可降低外周动脉疾病风险
2018-09-28 MedSci MedSci原创
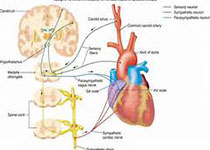
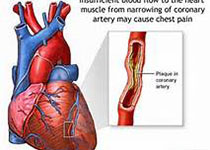
动物脂肪组织的海洋n-3多不饱和脂肪酸(PUFAs)含量被认为是机体长期摄入海产品的生物标志物。本研究的目的旨在评估机体脂肪组织中PUFAs的含量与外周动脉疾病(PAD)的关系。本研究纳入了丹麦饮食、癌症和健康研究队列中的对象,脂肪组织是从所有研究对象的臀部获取,经过平均13.5年时间的随访,共有870例对象出现PAD。分析结果显示,二十碳五稀酸(EPA)含量越高,PAD的发生风险越低([HR]:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
55
#ACC#
67
#疾病风险#
51
#外周动脉#
57
学习一下
122
学习了,涨知识了!
128