Cancer Res:王跃祥研究组发现克服胃肠间质瘤格列卫耐药新策略
2021-03-19 生物世界 生物世界
以伊马替尼(商品名:格列卫)为代表的靶向KIT/PDGFRA激酶抑制剂的临床应用,使胃肠间质瘤(GIST)病人的5年生存率已由2000年的15%提高到当前的65%,这一重大进展得益于KIT/PDGFR

以伊马替尼(商品名:格列卫)为代表的靶向KIT/PDGFRA激酶抑制剂的临床应用,使胃肠间质瘤(GIST)病人的5年生存率已由2000年的15%提高到当前的65%,这一重大进展得益于KIT/PDGFRA 驱动基因的发现及相应的靶向治疗,但几乎所有病人最终都会产生耐药性,耐药后如何治疗一直是GIST基础和临床研究的焦点和难点。
2021年3月16日,中科院上海营养与健康研究所王跃祥研究组在 Cancer Research 杂志在线发表了题为:Integrated Screens Identify CDK1 as a Therapeutic Target in Advanced Gastrointestinal Stromal Tumors 的最新研究论文。
该研究首次发现CDK1是伊马替尼耐药胃肠间质瘤(GIST)的进攻弱点,阐明CDK1细胞周期外的新功能,为克服伊马替尼耐药提供了新的策略及临床前实验数据。
研究团队首先建立了一系列激酶抑制剂敏感/耐药的GIST模型,通过全基因组系统筛选伊马替尼耐药GIST的潜在进攻弱点,CDK1 位于所有必需基因的前2位。对晚期和早期GIST的多组学测序数据分析,在三个中国GIST队列中发现了CDK1在约30%的晚期GIST中高表达,在早期GIST中几乎不表达。
体内、体外功能实验证明CDK1高表达的GIST呈现CDK1依赖,敲除CDK1抑制体内体外细胞生长和成瘤,促进细胞凋亡和衰老。
分子机制上,激酶CDK1直接结合其底物AKT(通过蛋白质组学筛选获得)并磷酸化473位丝氨酸和308位酪氨酸,从而促进GIST的增殖和进展,该分子机制也解释了晚期GIST中AKT高度磷酸化的原因。CDK1的小分子抑制剂RO-3306在CDK1高表达的GIST中显着抑制细胞增殖,而对CDK1不表达的GIST细胞则无影响。
在伊马替尼耐药的PDX小鼠模型中,CDK1抑制剂显着抑制肿瘤生长,证明CDK1抑制剂具有抗伊马替尼耐药GIST的活性。
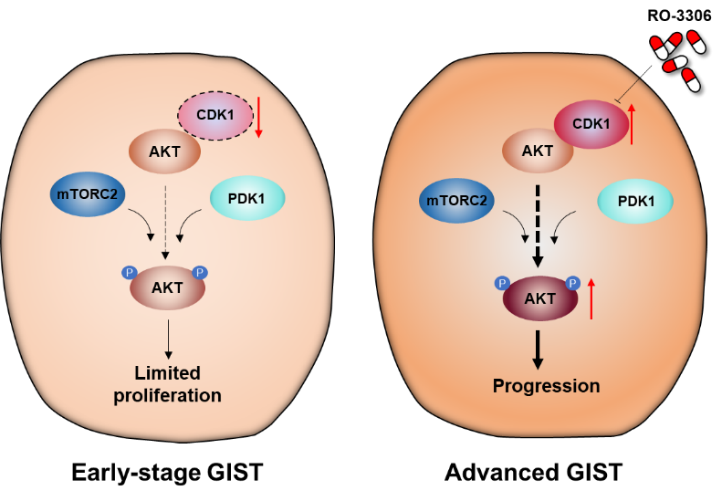
CDK1是伊马替尼耐药GIST的进攻弱点。(左)早期GIST中CDK1 不表达,肿瘤细胞的增殖能力有限;(右)晚期GIST中CDK1高表达,激酶CDK1结合其底物AKT并磷酸化473位丝氨酸和308位酪氨酸,从而促进GIST的增殖和进展。
该研究首次证明CDK1是伊马替尼耐药胃肠间质瘤(GIST)的进攻弱点,阐明CDK1细胞周期外的新功能及底物,提出CDK1驱动GIST的治疗策略,为克服伊马替尼耐药提供了新的策略及临床前实验数据。
据悉,中科院上海营养与健康研究所博士研究生芦晓晶、庞裕智、刘晓筱及上海交通大学医学院附属仁济医院普外科曹晖主任为该论文的共同第一作者。中科院上海营养与健康研究所王跃祥为该研究的通讯作者。该项研究也得到了上海交通大学医学院附属仁济医院胃肠外科屠霖博士和病理科沈艳莹博士以及我国台湾大学医学院Jen-Chieh Lee教授的大力支持。此课题研究得到了国家自然科学基金、科技部国家重点研发计划专项、上海市科委基础重点项目等的支持,也得到了上海营养与健康研究所公共技术平台、动物平台的支持。
原始出处:
Xiaojing Lu, Yuzhi Pang, Hui Cao, et al. Integrated Screens Identify CDK1 as a Therapeutic Target in Advanced Gastrointestinal Stromal Tumors. Cancer Research, 2021. DOI: 10.1158/0008-5472.CAN-20-3580.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#格列卫#
57
#间质瘤#
0
#新策略#
84
好文章!
106