CKD患者的血糖控制目标,哪些精髓不容错过?
2021-11-22 从医路漫漫 MedSci原创
美国糖尿病协会(ADA)推荐的非妊娠成人HbA1c目标为≤7%。其他患者的达标水平可以控制在<8%,如预期寿命较短、有严重低血糖史、较多并发症和晚期并发症的患者。
血糖控制良好可以减缓心血管疾病和慢性肾病的进展。美国糖尿病协会(ADA)推荐的非妊娠成人HbA1c目标为≤7%。其他患者的达标水平可以控制在<8%,如预期寿命较短、有严重低血糖史、较多并发症和晚期并发症的患者。HbA1c < 6.5%的目标可能只适合某些人群。美国临床内分泌学家协会(AACE)建议低血糖风险低的健康患者糖化控制目标HbA1c≤6.5%,但是仍需要个体化。
上述建议如何适用于慢性肾病患者尚不确定。2007年关于糖尿病和慢性肾脏病的肾脏疾病结果质量倡议指南认可HbA1c< 7.0%;然而,他们更新的2012年指南建议HbA1c约为7.0%。KDIGO(肾病:改善全球结果)举办的糖尿病肾病争议会议(DKD)指出,关于CKD期或更糟患者的理想血糖控制目标的临床试验数据不足。他们指出,接受肾脏替代治疗的糖尿病和肾衰竭患者从将HbA1c水平保持在7%-8%的范围内受益最大,因为HbA1c水平高于8%或低于7%会增加全因和心血管疾病死亡率的风险。如果患者没有服用任何可能导致低血糖的药物,可以考虑HbA1c<7%。护理的许多其他方面可能会影响血糖目标。

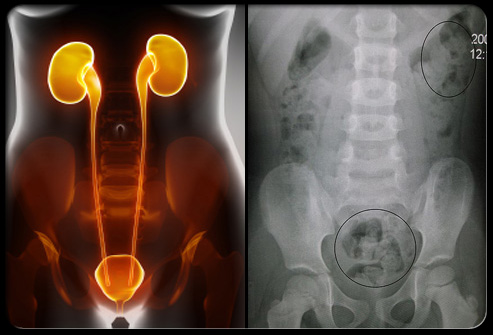
图 指导个人HbA1c控制目标的因素。缩写:CKD,慢性肾脏病;eGFR,估计肾小球滤过率;G1,eGFR≥90mL/min/1.73m2;G5,eGFR<15mL/min/1.73m2;糖化血红蛋白。
对于血糖控制稳定且达到目标的个体,应每6个月测量一次HbA1c水平;但是,如果血糖没有达到控制目标或治疗发生变化,应每3个月检查一次HbA1c水平。低血糖的风险随着肾小球滤过率的下降而增加,主要是在使用胰岛素、磺脲类药物或格列奈类的人群中。肾脏糖异生由于肾脏功能受损而降低,随着慢性肾病的进展,胰岛素和口服糖尿病药物的肾脏清除减少。与尿毒症相关的厌食和体重减轻也会增加低血糖风险。
当eGFR接近30mL/min/1.73m2及以下(4-5期慢性肾病)时,某些慢性肾病患者的HbA1c测量可能不准确。红细胞寿命缩短引起的贫血、溶血和缺铁都可能导致HbA1c降低。相反,出现血红蛋白氨甲酰化和酸中毒时,可以导致HbA1c升高增加。糖化白蛋白提示2周内血糖的波动情况。一些研究表明透析患者使用糖化白蛋白优于HbA1c,因为HbA1c低估了持续血糖监测(CGM)对维护性透析患者的血糖控制。然而,对于评估长期血糖控制,HbA1c仍然是首选方法,因为糖化白蛋白的准确性和实验室间变异性以及肾病综合征患者血清白蛋白水平特别低的问题仍然存在。此外,糖化血红蛋白反映了3个月的血糖控制,而糖化白蛋白仅反映了2周。当eGFR <30 mL/min/1.73 m2时,HbA1c的测量值比正常值低0.5%到1.0%。当胰岛素用于评估血糖控制和避免低血糖时,应每日多次测量血糖。
随着肾功能的下降,糖尿病的用药方案需要个体化。1型糖尿病患者需要胰岛素,可以设计多种胰岛素方案。对于2型糖尿病患者,有很多治疗方案和组合。因为慢性肾脏病患者对胰岛素和其他药物的清除率降低,患低血糖的风险更高。随着肾功能的下降,糖尿病药物可能需要经常调整。值得注意的是,一些药物可以减缓肾脏疾病的进展,比如SGLT-2。
原文出处:
[1]Hahr AJ, Molitch ME,Management of Diabetes Mellitus in Patients With CKD: Core Curriculum 2022.Am J Kidney Dis 2021 Sep 29
[2]糖尿病肾病防治专家共识(2014年版)[J].中华糖尿病杂志,2014,6(11):792-801.
[3]中国糖尿病肾脏疾病防治临床指南[J].中华糖尿病杂志,2019(01):15-28
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CKD患者#
67
学习了
82
#血糖控制#
68
#控制目标#
53
这个值得学习
84
学习了
91