【一般资料】
患者,女,12岁
【主诉】
因右臀部疼痛3天入院,疼痛以夜间为主,活动不加重疼痛。
【体格检查】
右臀部较对侧膨隆,局部皮肤正常,皮温略高,可触及一大小约4CM×3CM×1CM肿物,质硬,压痛,推之不动,髋关节活动正常。
【辅助检查】
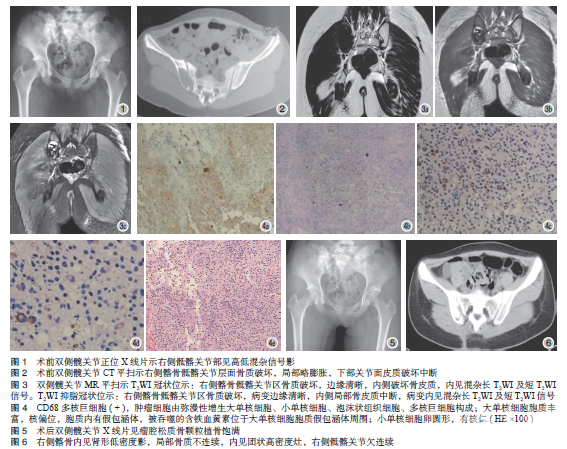
术前双侧髋关节正位X线片示右侧骶髂关节部见高低混杂信号影(图1)。双侧髋关节CT平扫示右侧髂骨骶髂关节层面骨质破坏,局部略膨胀,下部关节面皮质破坏中断(图2)。双侧髋关节MR平扫示T2WI冠状位示:右侧髂骨骶髂关节区骨质破坏,边缘清晰,内侧破坏骨皮质,内见混杂长T2WI及短T2WI信号。T2WI抑脂冠状位示:右侧髂骨骶髂关节区骨质破坏,病变边缘清晰,内侧局部骨皮质中断,病变内见混杂长T2WI及短T2WI信号(图3)。患者入院后行血、尿常规,乙肝五项,血生化,女性肿瘤标志物,血沉、C反应蛋白,心电图,胸片等检查,检查结果无明显异常。
【治疗】
于入院第2天行右髂骨细针穿刺活检术,取标本行病理学检查。病理检查结果:大体:灰红带骨组织一条,总体积约5mm×2mm×2mm,组织切面灰红、灰黄、质韧。CD68多核巨细胞(+),肿瘤细胞由弥漫性增生大单核细胞、小单核细胞、泡沫状组织细胞、多核巨细胞构成;大单核细胞胞质丰富,核偏位,胞质内有假包涵体,被吞噬的含铁血黄素位于大单核细胞胞质假包涵体周围;小单核细胞卵圆形,有核仁。免疫组化:LCA(部分+)、Vimentin(+)、S-100(组织细胞+)、CD68(组织细胞+)、CD38(-)、CD138(-)、Kappa(+)、Lambda(部分+)、Desmin(-)、P63(-)、CD1ɑ(-)、Ki-67指数(5%),病理学诊断:髂骨D-TGCT(图4)。全麻后行右髂骨近中线侧切口,逐层暴露至髂骨肿瘤部位,术中见肿瘤位于髂骨外侧皮质受侵蚀变薄,肿瘤侵蚀右侧骶髂关节,瘤体周围形成硬化骨窦,大小约4CM×2.5CM×1CM,边界不清,形状不规则,质韧。手术沿瘤壁外侧2mm完整清除肿瘤组织,用碘酊、无水酒精灭活瘤腔,并用蒸馏水浸泡冲洗后行同种异松质骨颗粒植骨。手术顺利,术后复查X线片见瘤腔松质骨颗粒植骨饱满(图5)。于2016年12月16日康复出院。术后半年(图6)复查髋关节CT平扫未见复发及转移。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腱鞘巨细胞瘤#
65
学习了谢谢分享!!
66
#弥漫性#
40
#细胞瘤#
55
#巨细胞#
54