Blood:JAK2抑制剂用于治疗骨髓增生性肿瘤(MFN)的效果和安全性评估
2018-04-13 MedSci MedSci原创
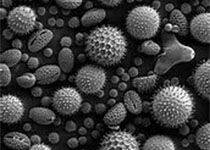
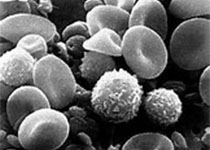
骨髓增生性肿瘤(MPNs)包括原发性血小板增多症、红细胞增多症(PV)和原发性骨髓纤维化(PMF)。在MPNs中可观察到JAK2。CALR和MPL基因发生表型驱动性突变,并可与额外的突变结合产生多样的表型。JAK2/STAT信号通路是MPNs的关键信号级联反应,驱动性突变可导致其构成性激活。卢索替尼(RUX),JAK2抑制剂(JAKis)的一种,已被批准用于治疗中高危的骨髓纤维化(MF)和羟基脲不
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JAK#
64
#2抑制剂#
68
#增生性#
59
#骨髓增生#
65
#抑制剂#
72
了解一下.谢谢分享!
87
#骨髓增生性肿瘤#
80
#JAK2#
110
学习了.谢谢作者分享!
95
骨髓增生性肿瘤(MPNs)包括原发性血小板增多症.红细胞增多症(PV)和原发性骨髓纤维化(PMF).在MPNs中可观察到JAK2.CALR和MPL基因发生表型驱动性突变.并可与额外的突变结合产生多样的表型.JAK2/STAT信号通路是MPNs的关键信号级联反应.驱动性突变可导致其构成性激活.
0